Healthcare Delivery System Reform, AEI Live Stream
Panel discussion at American Enterprise Institute November 2017 on Healthcare Delivery System Reform in the USA. Starts with lecture by Dr Brent James on Quality Science (slides posted at end).
PANEL
Brent James, MD - Quality Science
Elliott Fisher, MD - The Dartmouth Institute for Health Policy and Clinical Practice
Farzad Mostashari, MD - Aledade
Jeff Selberg - Peterson Centre on Healthcare
James C Capretta - AEI
Joseph Antos - AEI
The future of delivery system reform | Live Stream | American Enterprise Institute | 2:14 hrs
Summary
This panel is overall bullish on capitation or a virtual capitation models as a means to align incentives for better care with lower cost.
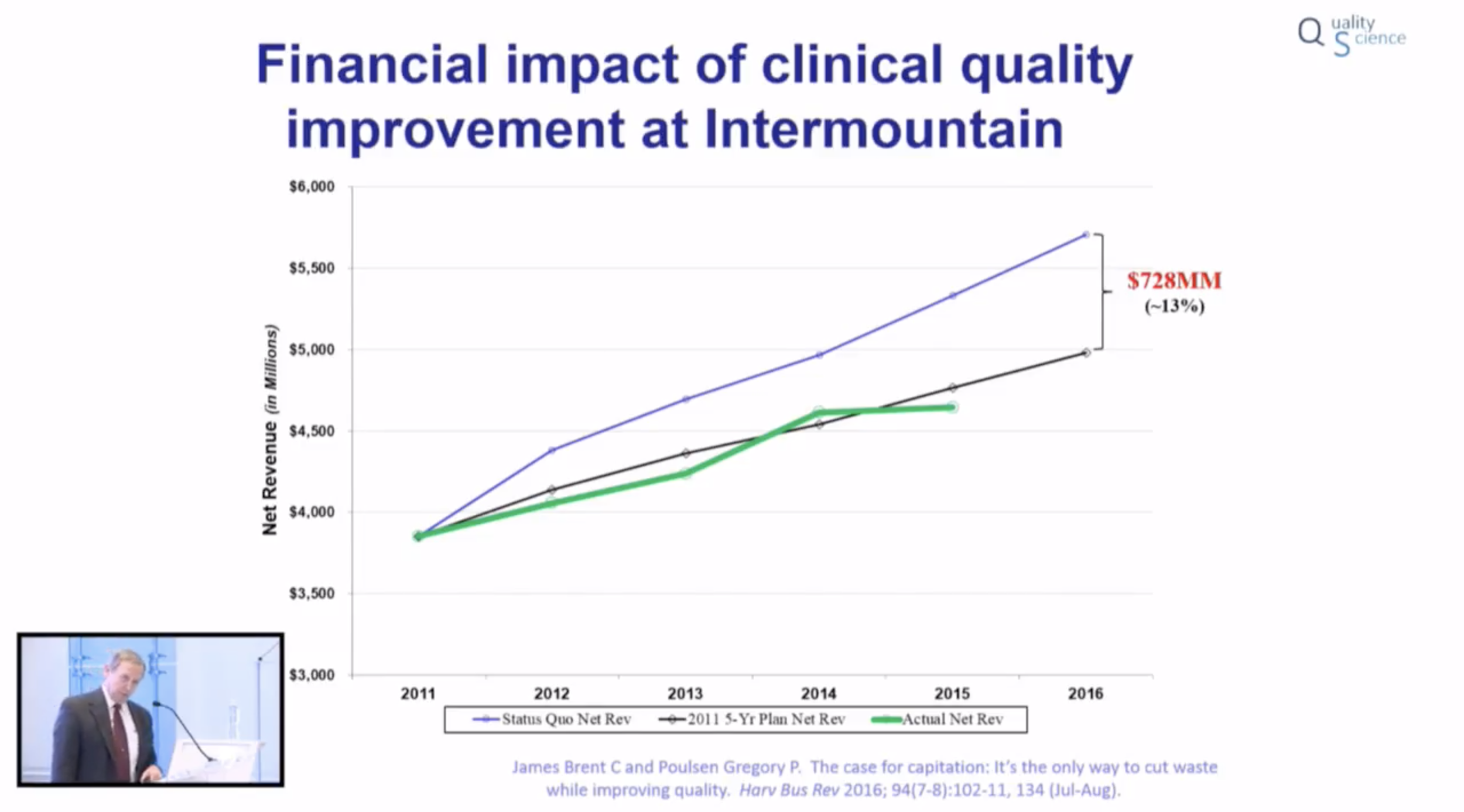
Improving the quality of care should reduce the cost of care, as higher quality services involve less waste in their production.
Like any conversation about healthcare in the USA, the financial bottom line is a significant driver of the discussion.
A few take away points
Brent James, MD - Keynote Presentation (slides at end)
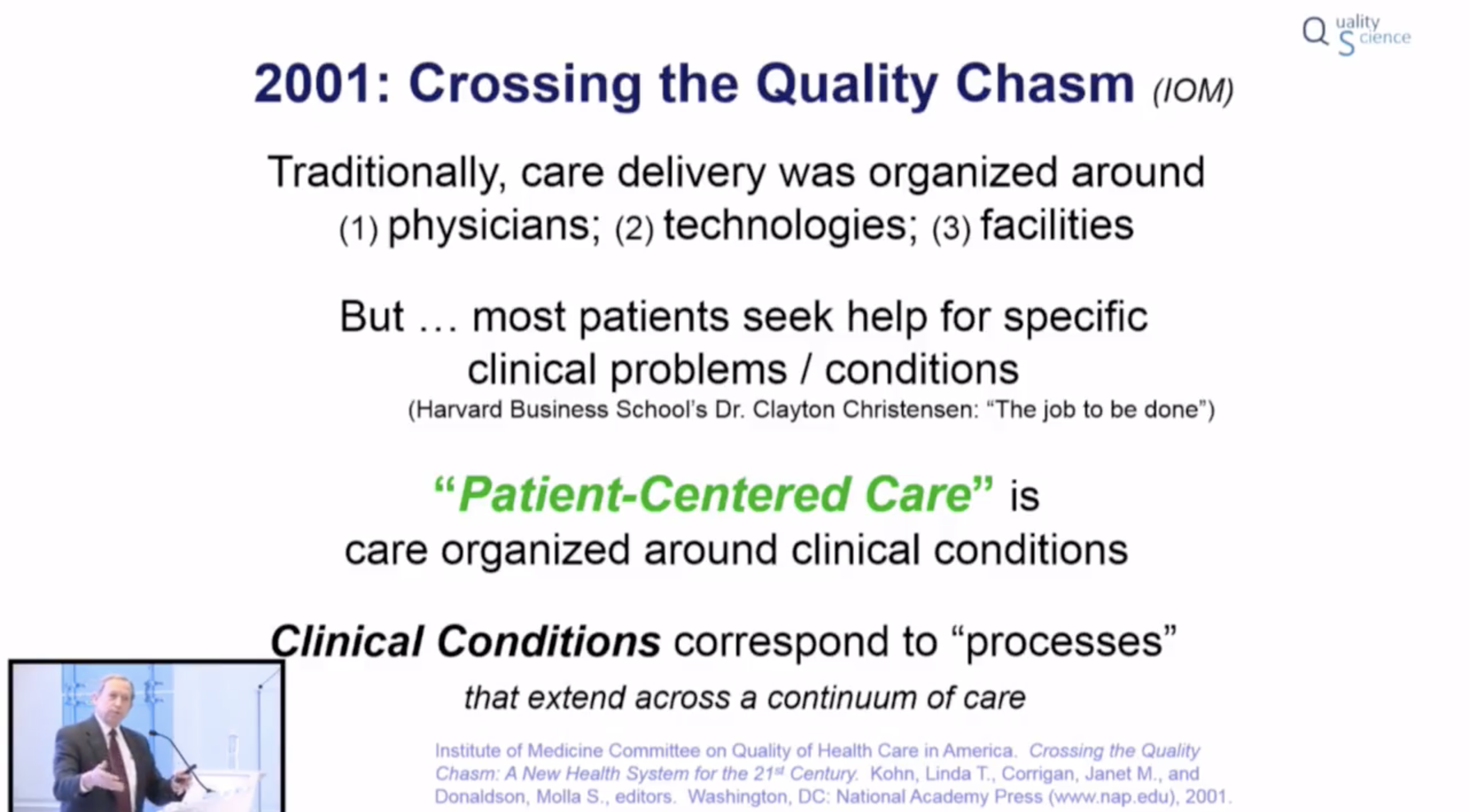
- Healthcare is arranged, and we cue up, patients around physicians, technologies, and facilities. When speaking of ‘patient-centered care’ the goal is to move the processes to be centred around the “job to be done” - the clinical condition itself rather than the pieces needed to tackle that problem.
- In one study, the care you received was more determined based on where you lived and the physicians you saw, than the level of insurance you had (or didn't).
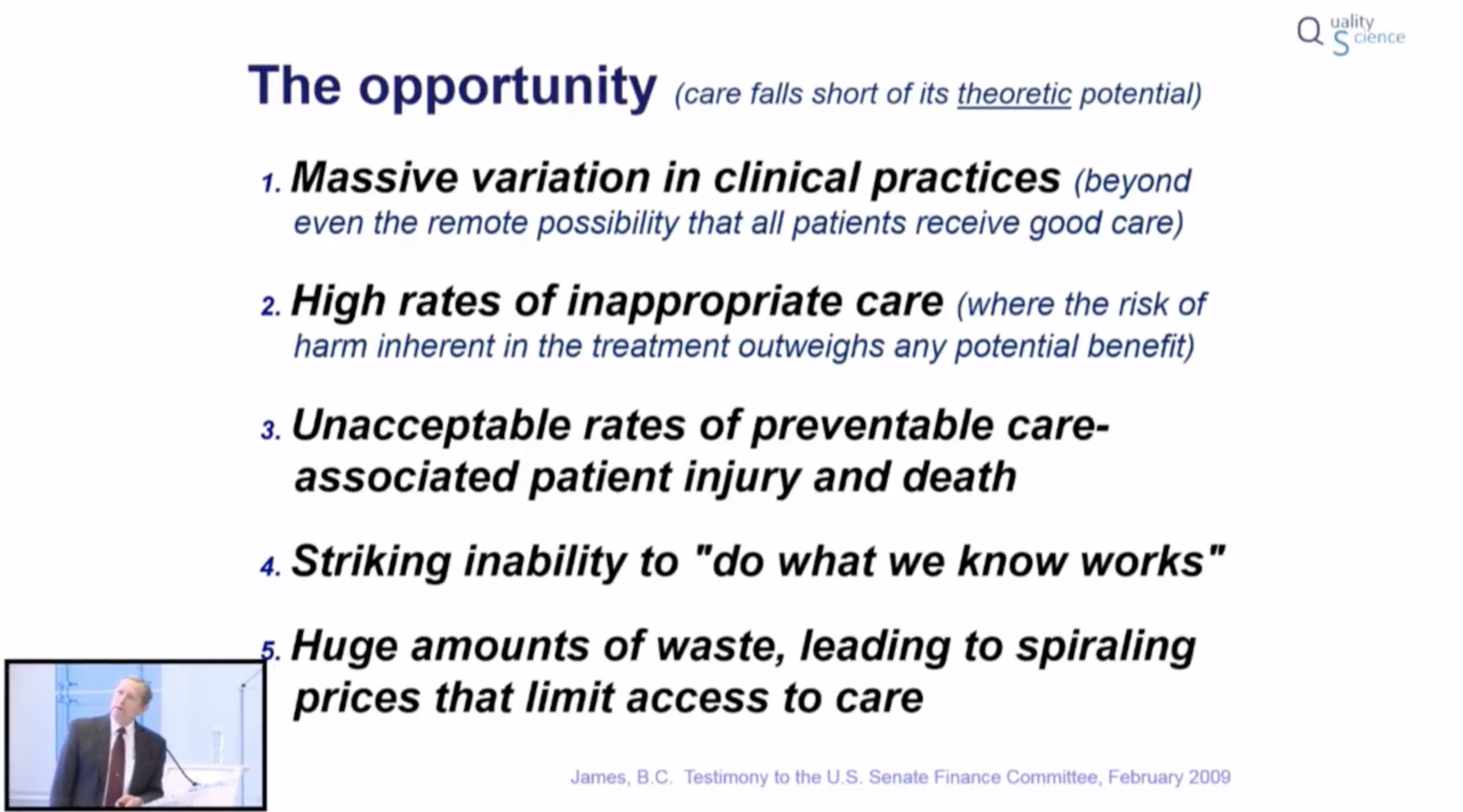
- The variation in care is so large, that even with full Gold Card access to care, it is impossible that a large number of people are getting good care.
- The closest ‘variation’ in care James found was 60%. The highest variation was 560%
- Variation in medical care is even higher outside of physicians, in areas such as nursing and physiotherapy.
- Multiple studies estimate that 30 to 50% of all healthcare expenditure is on ‘waste’. Dr James himself estimates the number closer to 70%.
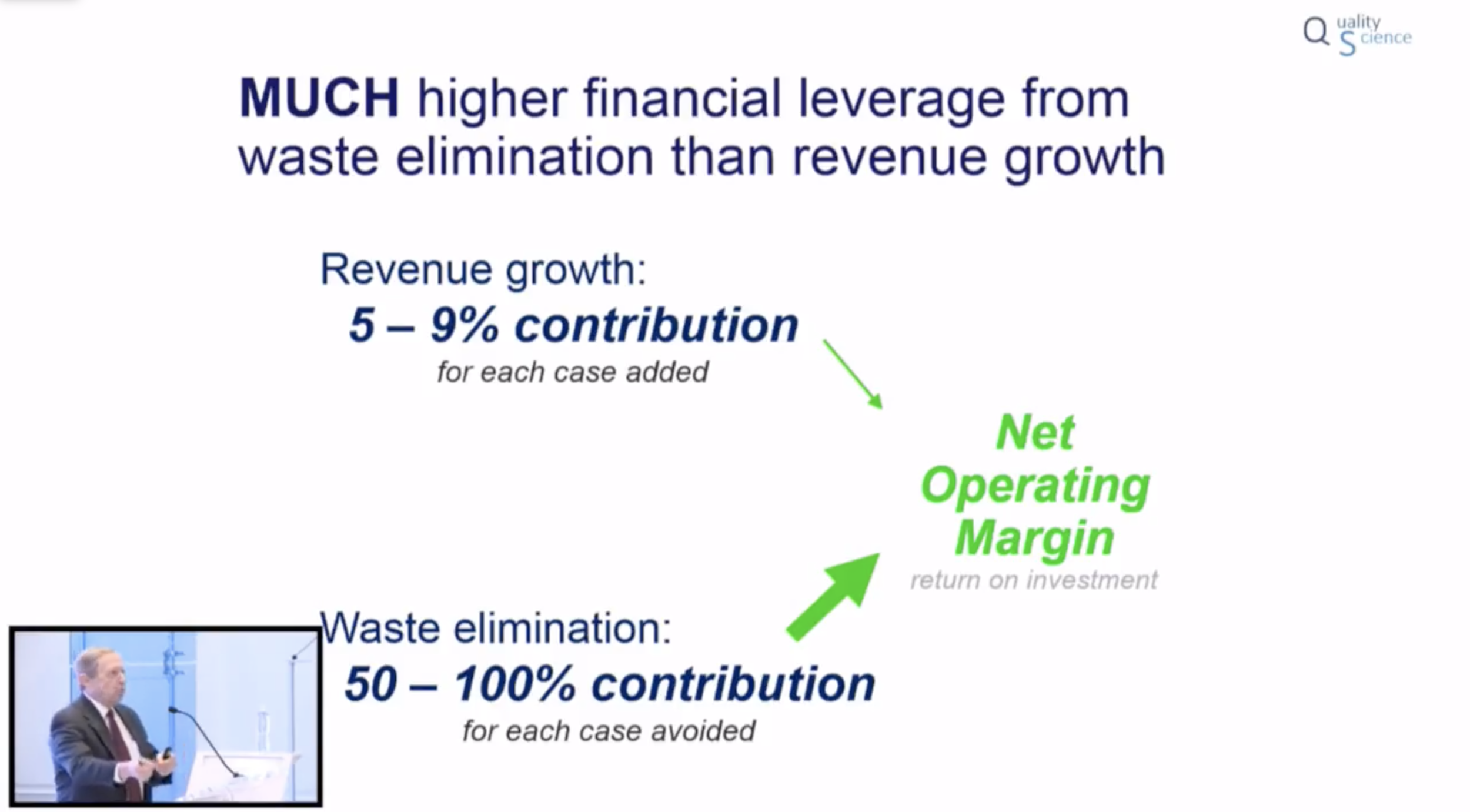
- Cheaper care through better care: The financial gains possible by targeting removal of waste from the system is multiple folds higher than one would make by focusing on traditional ways to ‘grow revenue’ (by expanding indications or new clients).
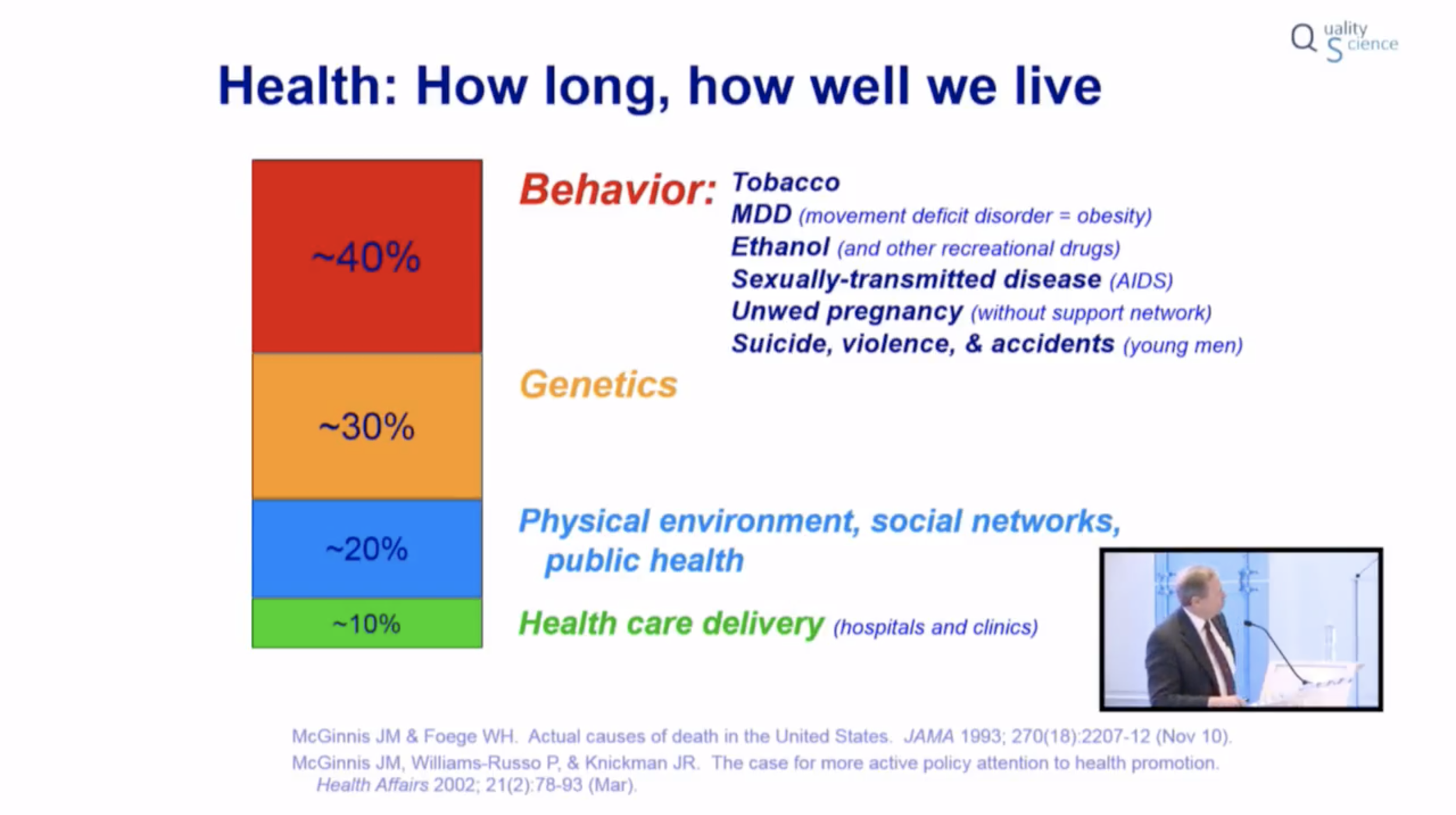
- Movement of care ‘upstream’ - aka closer to primary care and public preventative health is the best overall system cost control mechanism and method to improve healthcare outcomes.
- Anticipate the merger and convergence of insurance companies and care delivery systems
- Most patients do not pay any attention to rank tables of their physician or institution. Only 2-3% do. Instead, most choose based off their relationship with the provider.
- Physician incentives that show how they can provide better patient care, can have a greater impact on individual physician practice than financial incentives.
Elliott Fisher, MD
- Dr Fisher believes healthcare is premised on the lie that doctors can tell patients whats good for them. He believes in closer aligning healthcare's goals to the patient's goals
- The ACO model can improve hospital financials by providing better primary care to Medicare patients. These patients require less expensive downstream care later on. This will free up more beds in the expensive hospital - which can be used for higher revenue generating non-Medicare patients.
- Other capital intensive systems, such as airplanes and hotels separate the ownership of capital from the delivery of services. In healthcare this could mean that hospital beds and physicians would be separated. (Interesting idea: separation of capital ownership and service delivery...I need to think through this one in more detail)
Farzad Mostashari, MD
- As much as one can love public health initiatives, ultimately true system change comes down to incentives. If you want to improve public health, you have to improve the incentive structure.
- Moving towards site neutral payments is a way to help prevent escalating healthcare costs. Essentially preventing hospitals that buy outpatient practices from billing for the same service provided in that same facility now as a 'hospital' provided service with the associated uncharged hospital/facility fees.
- Push back, and be aware about the anti-competition trends seen with consolidation.
- e.g. Data blocking - not sharing patient care outside of their 'care network'.
- e.g. If you try to start a new healthcare plan in a market, the major hospital in that market holds disproportionate power. If they do not sign on with your health plan, you will essentially not be able to start your new plan in their market area.
Jeff Selberg
- If there is at least 800 billion dollars of waste in the healthcare system, it is the equivalent to what is spent on education in the country
- Goal of Peterson Centre on Healthcare is to identify where exceptional care is being delivered, isolate their systems of excellence, validate their models, and spread their methods.
- The exemplary medical practices (higher quality outcomes with lower costs) they encountered, did not know they were exemplary.
Critique
Shared decision making is discussed a few times as an important way to help aligning treatment decisions with the patient's goals, as well as create more customer driven market forces in healthcare. I don't disagree, this is a laudable goal. However, let us not underestimate how difficult this is to do at sale.
It is really hard to disconnect the biases of the physicians, their institution, and the patient's coverage plan from the decisions proposed to a patient that they can use to evaluate with their 'goals'. Especially when many patients do not actually have an articulable set of goals or values, and when they lack sufficient knowledge to weigh the medical choices placed in front of them. Not to mention, the decisions they are evaluating are intermediary medical choices - one does not really want a 'CT' or a 'biopsy' or a 'surgery'. They want the secondary outcome as a result of these interventions.
Ultimately, I believe a way forward is to create healthcare institutions that have such a strong level of patient trust in their 'brand identity' that patients can be assured their personal interests are always the organization's top priority.
Slide Deck
Brent James, MD
Keynote Presentation
Delivered at American Enterprise Institute (AEI), November 2017