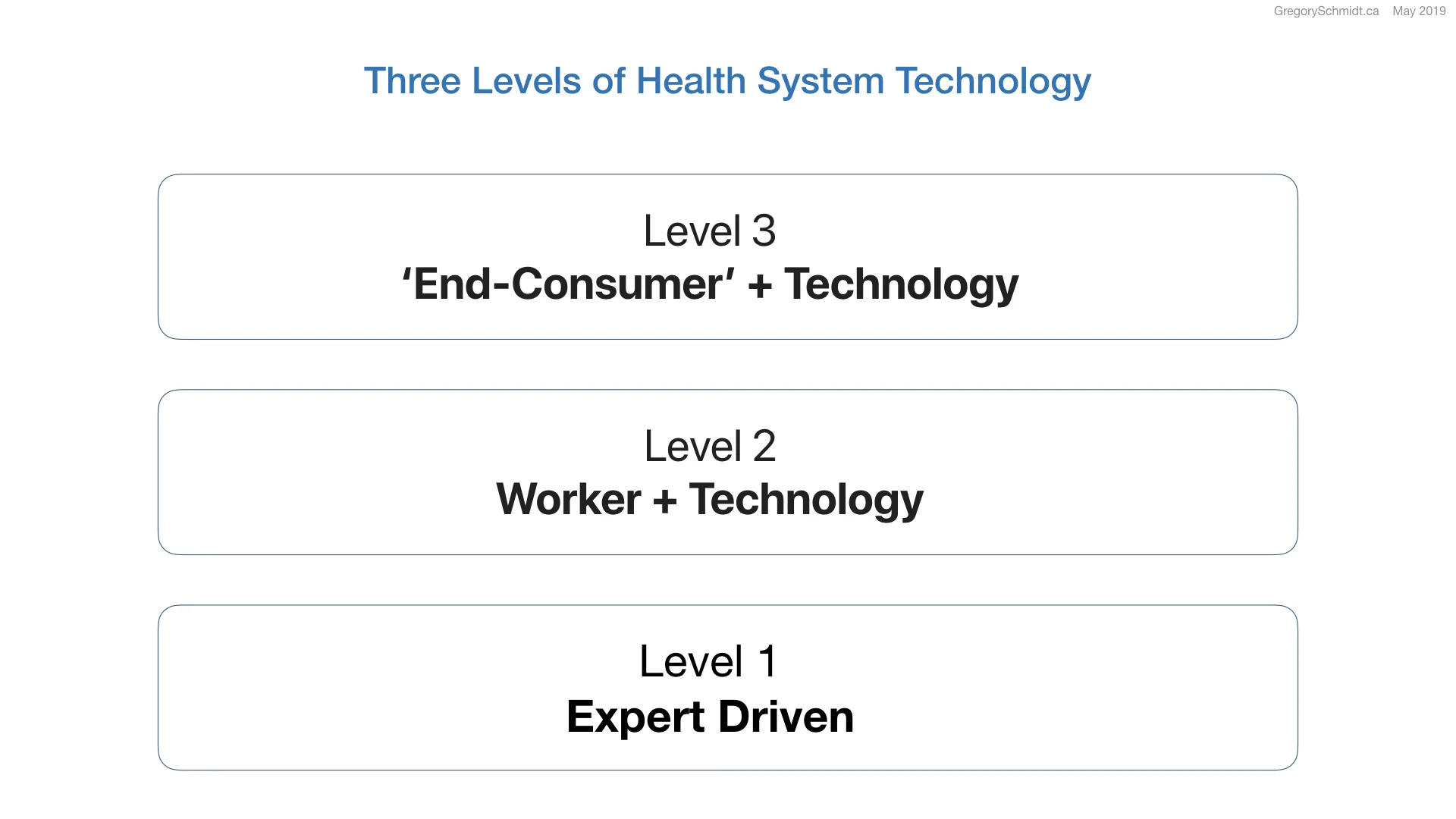
Three Levels of Health System Technology
This series on Health Systems Evolution looks at why technology and data systems play a critical role in being able to design & implement the next generation of healthcare systems.
This article looks at the move from Level 1 to Level 2 health systems: the shift from predominantly physician driven systems to systems where a significant amount of care is provided by (1) a healthcare worker, (2) using a digital health tool, (3) in an integrated system.
Listen to post as video below, or on your podcast app under: Gregory Schmidt
Three Levels of health system technology
To start, let’s discuss a well-known technology – booking travel tickets. At one time, if you went on a trip, you’d go to an expert travel agent. This person would have all the knowledge of which roads, trains, and ships were needed for travel. Let’s call this: Level 1.
Then there came a time when you went to a travel agent, and the person working there wasn’t a globetrotter guru, but a friendly and courteous travel agent who knew how to operate a computer. They entered your travel origin, destination, and preferences into the computer, and it would perform the cognitive work of suggesting several routes. Let’s call this: Level 2.
Today, if you want to book a flight, you’ll use the internet to a buy ticket. Or you may pull out your phone, and Siri can take you anywhere in the world. Let’s call this Level 3.
Technology enables people of all abilities to raise their skill set and to expand their competent scope of practice. At Level 3, the consumer can access the knowledge within the system directly; at Level 2 a competent user of the technology system is required to access the knowledge, and in Level 1 the knowledge is contained within the expert person – and so the technology is absent.
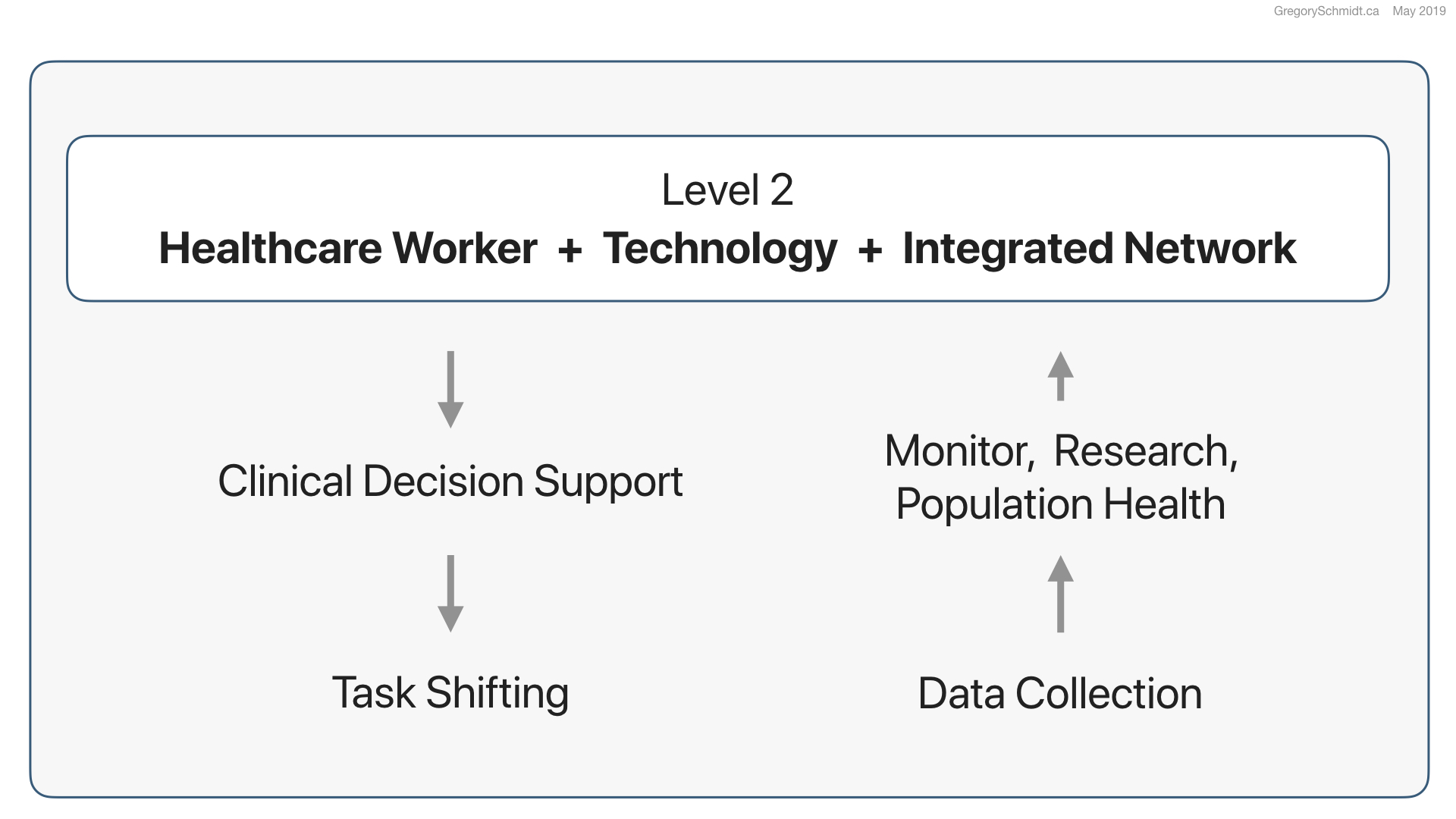
I believe, a significant step in healthcare system design is to move from Level 1 to Level 2 health systems. This moves away from Level 1 – where physicians predominantly deliver care, to systems in Level 2 where (1) healthcare workers are combined, (2) with technology, (3) in an integrated system.
Task Shifting
Level 2 systems enable task shifting to be done at scale. Task shifting is moving work that was done exclusively by physicians to other healthcare workers. The problem with physicians is that they are expensive and there is a significant worldwide shortage. Other healthcare workers take less time to train, are less expensive, and are more abundant. Task shifting changes how we consider the design of healthcare systems – and this is of particular importance in creating scalable health systems around the world.
Obviously not all work that doctors do can be task shifted. But I believe significant amounts of high value, routine care could be safely performed by (1) well-trained staff, (2) combined with the right technology, (3) working in an integrated system.
AMPATH’s HIV delivery network is built upon task shifting. We believe a core component in its success is the use of digital electronic health record tools directly at the point-of-care - running predominantly on mobile tablets. The digital tool becomes the link between the patient, the clinician, and the health system.
Lets look at three benefits of point-of technology that enable the move from Level 1 to Level 2.
a) Clinical Decision Support
One benefit of point-of-care digital health tools, is the ability to deploy clinical decision support to clinicians; such as care reminders, notifications, alerts, and suggestions. Decision support can help an outreach worker to have a higher skillset to care for people in their village with HIV, or it allows a nurse to provide more advanced hypertension care then they could without the digital tool to assist in care.
The hope with buzzwords such as machine learning and artificial intelligence, is that breakthroughs in these fields will help create algorithms that can provide even more advanced clinical decision support. This will then enable even more safe task shifting, and in turn expand the competent scope of practice of more healthcare workers.
b) Data Collection
In addition to knowledge distribution, these digital point-of-care tools also enable more reliable data collection compared to their paper alternatives. This is important to be able to monitor health systems to ensure they are working, to do research, and to study population health.
c) Integrated Networks
A caution: these tools work best when used in an integrate network. This network that provides pathways to (1) higher and lower levels of care, and (2) other care providers and services. If used in isolation, these tools loose their potency, and can lead to more dangerous and fragmented care.
Not a digital data vault
For too many years, the electronic health record has been viewed as a digital filing cabinet - a digital vault to store and retrieve data. But, it is better to view it as a conductor, that helps coordinate and orchestrate the many individuals involved in the healthcare system.
This makes the electronic health record more of a road network that distributes knowledge & clinical decision support, and then collects back data for monitoring and evaluation.
This leaves the role of the electronic health record as a quarterback in the care system.
This is a high level ambition of where our digital informatics tools need to move to, in order to be able to have the tools needed to build the next generation health systems we require.
Leapfrog
I think all of this is particularly exciting because just as many countries leapfrogged over land-lines, directly to cell phones, I wonder if many countries may leapfrog over Level 1 healthcare systems, to Level 2 systems; that are theoretically more efficient, effective, lower cost, and scalable - through the ability to combine technology with health workers, within an integrate healthcare delivery system.