Exponential Medicine, Day 2 - Cool Stuff Summary (Nov 5 2018)
This is a collection of the cool ideas that I’d like to reference again in the future.
I wasn’t able to attend Exponential Medicine this year, but enjoyed watching the live stream from Kenya.
You may be interested in the notes from Day 1, Notes from Day 3, or Notes from Day 4
This post is available as a video (below), or on podcast app in audio under: Gregory Schmidt
Day 2 - Presentations
Monday, November 5 2018
Session 6: On the Frontier of Biotech
6.1 Moira Gunn PhD Host, NPR's Biotech Nation and Technation Health
6.2 Andrew Hessel CEO, Humane Genomics and Nanotechnology/Biotechnology Faculty, Singularity University
6.3 Jamie Metzl JD PhD Author of Hacking Darwin: Genetic Engineering and the Future of Humanity and Senior Fellow, Atlantic Council
Session 7: Digitizing Data, Health & Life
7.1 Ran Balicer MD MPH Director, Clalit Research Institute
7.2 Lonnie Rae Kurlander Founder & CEO, Medal
7.3 Poppy Crum PhD Chief Scientist, Dolby Laboratories.
7.4 David Karow MD PhD CEO, Human Longevity, Inc.
Session 8: AI for Good: Clinical Acceleration
8.1 Rachel Thomas PhD Founder & Researcher, Fast.Ai
8.2 Alan Karthikesalingam MD PhD Google Deep Mind
8.3 Johann Fernando, PhD Chief Operating Officer, FujiFilm Healthcare
8.4 Rajeev Ronanki SVP & Chief Digital Officer, Anthem
Session 9: Reimagining Regulation & Clinical Trials
9.1 Asif Dhar Principal, Deloitte Consulting LLP
9.2 Ashish Atreja MD MPH Chief Technology Innovation and Engagement Officer, Icahn School of Medicine at Mount Sinai
9.3 Hansa Bhargava MD Senior Medical Director, WebMD and Host of Medscape's Uncharted Medicine
Session 10: Smart & Healthy Communities
10.1 Lucien Engelen Founding Director of REshape Center, Radboud University Medical Center / SUNL
10.2 Erik Gerritsen Secretary General, Ministry of Health, Welfare and Sport of Netherlands
10.3 Elizabeth Canis VP Strategic Initiatives, Anthem
Session 11: Digital Surgery
11.1 Shafi Ahmed Professor of Surgery and Associate Dean, Barts Medical School
11.2 Carla Pugh MD PhD Professor of Surgery Stanford
11.3 Jean Nehme MD CEO and Co-Founder, Touch Surgery
11.4 Stefano Bini MD Professor of Orthopedics, UCSF
Session 12: It's All About Timing: Health, Aging and Interfaces
12.1 Leerom Segal Co-Founder and CEO, Klick Health
12.2 John Brownstein PhD Chief Innovation Officer, Boston Children’s Hospital Professor, Harvard Medical School
12.3 Satchidananda Panda PhD Professor, Salk Institute for Biological Studies
12.4 Jeffery Bleich Founder and CEO Pulson
12.5 Julia Vishnepolsky MA LMHC R-DMT Expressive Arts and Dance Movement Therapist, Adult Day Health Care
Session 13: Curing the Incurable
Jack Kreindler MD Founder & Director, The Centre for Health and Human Performance
Parker Moss Health Technology Entrepreneur in Residence, F-Prime and Eight Roads
Session 14: Connecting the Dots: Solutions at Scale
Rasu Shrestha MD MBA Chief Innovation Officer, UPMC Executive Vice President, UPMC Enterprises
Session 6: On the Frontier of Biotech
6.1 Moira Gunn
PhD Host, NPR's Biotech Nation and Technation Health
Biopharmaceuticals is new and growing industry. These are drugs made from a biological source, such as blood products, hormones, immune factors, vaccines, monoclonal antibodies, gene therapy, [wikipedia]
The Biopharma pipeline:
Highly innovative industry: “74% of biopharma compounds in clinical development are potentially first-in-class medicine” (meaning no previous drug designed to address that problem).
“Of the 850 new therapeutic products approved between 2000 and 2011, only 4% were indicated for neglected diseases.” - Lancet, 2013
‘More than 1 billion people….suffer from one or more neglected diseases’ - WHO
DNDi - Drugs for Neglected Disease Institute
Difference between biotech vs synthetic biology. Biotech involves cutting and pasting of DNA, whereas synthetic biology involves printing of whole molecules or organisms.
6.2 Andrew Hessel
CEO, Humane Genomics and Nanotechnology/Biotechnology Faculty, Singularity University
What is the relationship between biology and carbon? Are cells ‘mini-computers’ and ‘3D printers’ (they make more of themselves). How do we move from chemical world to DNA world?
Cost of DNA sequencing was following Moore’s Law from 2000s until 2008 when next generation sequencers were produced and then the cost fell exceeding Moore’s Law.
Today DNA sequencing today has become….Free.
Roswell chip should be able to sequence DNA ridiculously quick and at minimal cost [website]
Recently, Andrew has become fascinated with this graph showing in red the drop in the cost of genetic sequencing, and in green the ability to actually extract value from the genome that was sequences. We have now passed this economic inflection point.
This means that genomic companies have gone ‘exothermic’ - they get more economic value from the data from the genome than the cost to sequence the genome. Therefore - the more people you can sequence the more valuable your company becomes.
eg. of Companies trying to network genomic companies and patients together: It is kind of like having a wealth manager - who helps you extract value from letting other people have access to your genome.
[Admittedly, this sounds pretty close to Gattaca]
Not just people: eg. Earth Biogenome Project - aims to sequence genome of all eukaryotic’s on Earth in next decade.
Digital DNA to chemical DNA- ‘Synthetic biology’
Twist Bioscience - went public last week, create synthetic DNA (though just shorter strands)
Next is to use enzymes to assemble DNA. Companies doing this eg. DNA Script, Molecular Assemblies, Nuclear Nucleics.
Ginkgo Bioworks - ‘The Organism Company’ - creating biology for manufacturing / other industries
Genome Project - Write (GP-write) is the second half of the Human Genome Project. This first half was to sequence the human genome. The second half is to be able to treat any genetic disease. But in order to do this one needs to be able to write genomes. GP-write is a non profit working on genetic synthesis.
This means we can do, N-of 1 Medicine: ability to create medicines that are unique to you. As discussed yesterday eg. of Kymriah (human T cells). Cost to produce will fall as cost of genome sequencing did.
Creating viruses for dogs is very easy to do, and very cheap.
The good, ‘the app store for humans’ is opening up
The bad. This is incredibly scary. “Biosecurity needs an upgrade”.
Hacking Humans: IVF, IVG, CRISPR,
Garage biology can be done for a few thousand dollars, and soon all you will require is a laptop.
6.3 Jamie Metzl
JD PhD Author of Hacking Darwin: Genetic Engineering and the Future of Humanity and Senior Fellow, Atlantic Council
New book: Hacking Darwin: Genetic Engineering and the Future of Humanity
Where are we heading with the genetics revolution?
Watson / Crick - there is a book of life
Human Genome project - how to read the book of life
Next (CRISPR, etc) - how to write the book of life
“Human beings are another form of information technology”
From interview at break: people will be able to program biology, the same way people were programming apps. This is already happening. The software required to design biology is improving and becoming more modular, and the printers are getting better.
When he designs organisms, adds barcodes into DNA so that its possible to know who produced it. Advocates for a central registry for synthetic biology.
Creation of massive human DNA data pools. eg:
UK: NHIS plan this year to sequence 5 million Britains over next 5 years [news release]
US: All of US plan 1 million people [news release]
China: goal to sequence half of all newborns by 2020
Interest to compare DNA records from physical medical records/EHR.
“Healthcare is just a station along the way to our genetic future”
We are in the early phase of direct to consumer genetic testing. It is almost bogus at this time.
“The real destination will be in embryo selection”.
All that is knowable at ths timeis a few single point mutation disease, hair color, and eye color. But our ability to select will become increasingly better as prediction increases as a result of our knowledge from large human DNA pools
Fertility Clinic 2035
Week prior someone takes skin graft. It may not have to be sperm or embryo, for instance, recent research shows how to female rats can be mated with each other - there are multiple ways to generate these embryos.
‘This embryo will have Down’s Syndrome. This embryo will have a 50% chance of an outgoing personality’
Embryo mating: can mate people who have created their own embryos with each other.
The benefits of gene editing, likely will be very small compared to what can be done by embryo selection.
Jamie makes passing comment at end that this raises ethical questions, and we will require discussion on what norms and regulations are required on a global global level, just as there are global norms on biological weapons (1972), chemical weapons (1993), land mines (1997), cluster munitions (2006), and nuclear weapons. [I am very skeptical China would sign onto anticipated genome regulations]
[EDITORIAL: This is by definition Eugenics - "a set of beliefs and practices that aims at improving the genetic quality of a human population.” (Wikipedia).
We need to have an honest discussion about these technologies. If people want to advocate for them, they have to stand by advocating for eugenics. Or make the argument that, ‘this time is different’. Lets not whitewash the discussion.
As we create new ‘technologies’ people assume that because we can do something with technology, that we should do something with it. From what I have seen, not enough consideration given to the implications, consequences, and unintended consequences of the technologies we create.
The prevailing ideology is that, if it can be done, it should therefore be done.]
Session 7: Digitizing Data, Health & Life
7.1 Ran Balicer
MD MPH Director, Clalit Research Institute
Some facts: 30% of care is futile. 45% of necessary interventions are missed. The #3 cause of death is medical errors. We need to do better.
At Clalit in Israel, they have 20 years of EHR data available on 4.5 million patients. (They have their own EHR system)
Data can be used for Pre-emptive care. The goal is to predict a heart attack. But today using it to predict who will require dialysis (in order to intervene), or who is at risk of fracture.
I-deal Health: how a patient can understand their health, and how interventions they make will influence their health. Helps them understand how to make health choices better and “visualize their own success”
Clalit looked into the data from the NEJM SPRINT Data Analysis Challenge (hypertension trial). For each individual patient in that cohort they calculated the benefits and risks associated with intensive treatment. [NEJM - Winners]
And although the trial showed that ‘the average treatment effect’ was positive. When they calculated the individual patient’s risks and treatment benefits, they found that more than half of the patient’s in the trial should not receive the treatment. This moves from ‘average treatment effect’ to understanding ‘personal treatment effects’.
The fourth slide shows a patient risk calculator anyone can use using this data. For this work, they one first place in the NEJM data challenge.
Patients can then have their personal preferences for risk of each condition inputed, and these weights change the outcome of the recommendation.
This is how we embed patient’s preferences in the algorithms.
“Health systems will not be replaced by algorithms”
However, health systems that do not use algorithms will be replaced by those who do”
‘Physicians don’t require more data. They require data brought to them at the right time, and in a way that it can be actionable.’
7.2 Lonnie Rae Kurlander
Founder & CEO, Medal
After she was hit by a bus, she started creating spreadsheets of her own care.
This experience, combined with difficulty getting access to her own patient’s data as a medical student led her to found Medal - a tool to extract clinical data from EHRs.
‘Move from treating individual problems to managing lifelong disease.’
‘We are no longer detecting people who have heart failure. But people who have a propensity to develop heart failure.’
Over 130 different EHRs on market.
“When information matters most in healthcare - we resort to paper and fax” There are an estimated 15 billion faxes a year. Small hospitals receive 30,000 pages a day.
“In healthcare if you’ve seen one implementation [EHR], you’ve seen one implementation. Everyone one is different”
Semantic vs Syntactic Web.
Some screenshots of Medal.
Presentation ends with story of how she developed Ehlers-Danlos syndrome, and did extensive research into her own care, genetics, and help find treatment.
7.3 Poppy Crum
PhD Chief Scientist, Dolby Laboratories.
Francis Bacon artist, likely painting the world as he perceived it through a visual field distortion from a scotoma.
The devices around us in our homes, will know more about our emotional and mental state than the physician in the clinic.
“Our bodies can give off deterministic signals”, even if we try to hide them.
Even the diameter of your pupil. “Your pupil doesn’t lie” In the past pupil tracking technology was $20,000, but it is being shrunk and decreased in price to be in the smart devices in your house and mobiles. [AR will use pupil tracking a fair bit]
[….this sounds like Blade Runner….]
Galvanic Skin Response does not lie. Chart below shows how it can perfectly be predicted as humans watch penalty kicks.
Faces give off thermal changes, based on if people are engaged, or under stress.
The chemical composition of people’s breath changes in real time. This graph below shows how it changes as people watch The Hunger Games.
Proposal: we are leaving the era of the poker face; and entering the era of the empath.
The ear becomes the bi-directional access to our inner state:
The homunculus of today, and in three years from now will continue to change. (eg. our thumbs now have a larger proportion from texting).
The human’s ability of “plasticity is one of our most powerful tools” because it allows us to adapt and use the new technologies being developed that target our sensory experience.
7.4 David Karow
MD PhD CEO, Human Longevity, Inc.
The advancements in genetic sequencing from a decade prior still hadn’t reached clinical medicine. Which was part of the catalyst to want to start Health Nucleus.
Therefore they put people through all body phenotypic measurements available at the time.
The results from “healthy” clients were shocking. Remember, these were people who had been to executive physicals at places like Mayo Clinic, Cleveland Clinic and were told there they were ‘healthy’.
(remember, these findings could have been found through a superficial sensor or watch)
Some case studies:
40% left with a new ‘clinically significant’ finding. Many of which were actionable.
Important to remember genetic findings often do not only benefit the patient, but are valuable to their family members too who may be at risk.
Meaningful extension of life
Problem: 1/3 people who live to age 50 do not live to age 75 because of preventable premature mortality from chronic age related disease.
The goal is that by using this information from multiple sources, a personal risk prediction score for that person can be designed, and then provided to the patient with specific recommendations on what variables they can change to reduce their risk - and the effect of these interventions on their risk score.
The scalable & meaningful data required precision medicine:
True assessment of your code - genetic sequencing (not just asking a family history)
True assessment of your core - whole body MRI (not just doing some external physical exams)
David predicts that everyone at age 40 will undergo a whole body MRI to help guide ‘decision support’.
Session 8
AI for Good: Clinical Acceleration
8.1 Rachel Thomas
PhD Founder & Researcher, Fast.Ai
Founded fast.ai in order to help make it easier for anyone to learn how to use latest tools in AI. Have had over 200,000 students take their intro class.
Some work from their students:
Myths about AI
1. You need big data: using transfer learning, can create system with even 30 or 1000 images
2. Deep learning only works for very limited problems: computer vision is popular now, but other data such as tabular data, time series, text.
3. You need expensive computing power: you can often rent one in the cloud for 40 cents an hour, and for their course you often need about 70 hours of cloud domain.
4. Deep Learning replaces domain experts: domain experts really required to understand problems of how AI is interpretation data sets.
5. You need (to hire) a deep learning PhD from Stanford: the people working in your organization and already with your data can learn these skills.
8.2 Alan Karthikesalingam
MD PhD Google Deep Mind
Despite Google’s engineers building their data centres with incredible care and thought, when they applied AI to the management of the centre’s energy, they were able to reduce energy usage by up to 40%.
Challenges in health systems globally
Q: Can AI help us stop preventable sight loss?
Affects about 300 million people around world, and 80-90% of it is preventable.
Gold standard is OCT - optical coherence tomography of retina.
Published their results from their AI system reading OCT images in Nature September 2019. Demonstrating ability to classify for referal 50 eye conditions better than ophthalmologist and did not miss an urgent case.
To get around the black box problem, their solution splits the problem into two parts. First, the AI colors the layers of the retina, and the flickering of the red area suggests there is higher uncertainty with that area - thereby the physician can choose how they want to interpret the AI’s assessment of the scan.
These tools can be used for medical education, by having the user draw the areas they think have fluid in the eye, and then show where the algorithm is seeing fluid.
The training data sets can be small as 650 images:
Next
Trying to use these techniques on imaging for screening breast exams. In the UK two physicians are required to read each of these images, and all women age 50+ are invited to be screened. Leading to large costs.
Working with Veterans Affairs to develop algorithms to detect clinical deterioration in hospitalized patients before it happens.
How the results from the algorithms get into the clinical workflow will be critical.
Patients involvement is at the heart of all DeepMind projects.
Goal for 5 years from now: AI is not something ‘out there’, “but a routine tool in medicine. Subject to the same peer reviewed evidence that clinicians and patients can feel comfortable with”.
FujiFilm Healthcare
Johann Fernando PhD Chief Operating Officer, FujiFilm Healthcare
FujiFilm’s healthcare portfolio:
REiLI - FujiFilm AI’s platform [website]. They are building this platform as a tool to incorporate AI tools (both 3rd party and by FujiFilm) into radiology PACS workflows. In essence spanning an interoperability function as well as workflow function.
[The video below demonstrates in more detail how this works]
They have project working on sarcopenia detection - I suspect customers will pay $$ for this.
8.4 Rajeev Ronanki
SVP & Chief Digital Officer, Anthem
How AI is being used today: (1) Process Automation, (2) Insight Generation, (3) Personalized Engagement
How these can be combined:
AI Gone wild (and how these risks can be minimized)
Session 9
Reimagining Regulation & Clinical Trials
9.1 Asif Dhar
Principal, Deloitte Consulting LLP
As software becomes larger in healthcare, how does regulation of it work? The way that hardware and physical goods are regulated does not work in software - given software process of quicker updates.
In part because of the conversations at Exponential Medicine, the FDA has been moving to a software precertification program.
New class, ‘Software as a Medical Device (SaMD).
The new process can be streamlined to quantify how risky the software is, and also how much data it will share back to assess its real world performance. Those that are low risk + share most real world data can be fast tracked.
Comparable example. Those who share data with fast track for US border crossing, are able to cross faster, because we know their risk is lower.
Getting this new regulation work completed in a timely manner is important. Otherwise we will loose those developers who want to work in healthcare, to other fields if they realize that healthcare is too slow and difficult to work within the software regulation.
9.2 Ashish Atreja
MD MPH Chief Technology Innovation and Engagement Officer, Icahn School of Medicine at Mount Sinai
About Mount Sinai
There is now a business driver to keep people out of the hospital. And this creates a business driver to try new tools and technologies in IT.
Need to go beyond the EHR.
eg. First FDA approved app. 2001. in RCT showed a 1.2% A1c decline compared to usual care over 12 months. (eg. same decline as a billion dollar drug).
eg. AI driven text messaging tool reduced LDL-C, blood pressure, BMI, and smoking.
eg. Digital biomarker for smoking, based on sensor motion.
eg. FDA approved pill with sensor to track when it is ingested and then defecated.
They’re vision of care for 2020 (within 2 years)
Challenges: 78% patients want digital tools for health, yet 2% of providers recommend them.
Need new science of: EBDM - Evidence-Based Digital Medicine
They have grown to create the largest health technology validation network, so that within nine months you can produce the evidence required to show to the FDA.
Building a digital integration ecosystem:
Very fast patient recruitment
Goal is to create a platform where the right digital tool can be prescribed to patients depending on where they are in a care plan.
9.3 Hansa Bhargava
MD Senior Medical Director, WebMD and Host of Medscape's Uncharted Medicine
Problem: US maternal mortality is rising
WebMD 76 million unique monthly users (74% mobile).
Pregnant women, 55% download health apps.
To help work on this problem WebMD worked with Scripps. Used research kit on the PowerMom WebMD App (used by 1 million people). Their study findings:
Break
Discussion with Stefano Bini, MD
Interesting observation, Stefano mentioned he used to complain a lot about the electronic healthcare records [this is true, we’ve shared many long rants about EHRs over the years].
However, new insight was that in addition to EHR companies not wanting to share data, hospital systems do not want to share data. Because it means their patients may be able to go to another hospital system easier.
Robotics - has potential to reduce variability in surgery, which means outcomes will be more certain.
10. Session 10
Smart & Healthy Communities
10.1 Lucien Engelen
Founding Director of REshape Center, Radboud University Medical Center / SUNL
Sometimes healthcare in the Netherlands feels like they are on a different planet, as he is lucky to work in a country where their healthcare system is ranked for 7 years in a row as the “best in European Health Consumer Index EHCI”.
Though in many places “We need to take a day off, to burn fossil fuels, to drive to the hospital, to get the last parking spot, to rush to the front desk, where you are told ‘He is running late, take a seat’…Eventually you are called in, and your 8 minutes, and burn fossil fuels to get back"
Digital Human avatars - to change our ideas of healthcare.
The most important conversation we need to be having about changing healthcare is about culture. It is needed more than technology, leadership, or strategy.
Years to reach 100 million people: air-travel (70 years), telephone (50), PC (14), internet (7), Facebook (4 years), Instagram (2 months)
Healthcare is being debated, at tables we are not at the tablet at. Chart below shows non-traditional companies that have made healthcare announcements of over $10 million in last year.
Healthcare user experience (H-UX) is broken. Compare it to other sectors and fields.
The Copernican moment: healthcare previously circled the professional, and it is being shifted to circle the patient.
“Digital strategy is not translating what you do now digitally. It is completely rethinking your model grounds-up” [We have not approached digital healthcare with this mindset over the last few decades, from my perspective, we just replicated what we did in analog world, into digital work]
Predictive analytics are going to dramatically change healthcare - given that now we are reactive.
Half an hour before a patient is going to become hypoglycaemic they can now predict this and avert it.
Digital first, physical next
In 1960s stock exchange was men standing in room shouting at each other. Now only 3% of stocks are exchanged verbally, the rest is automated.
Comparable example today, is that a single ICU nurse can remote monitor from a computer 250 patients in real time. ‘Healthcare will become a software branch’.
Three phases of innovation: awareness, groundwork, execution. Today we are finishing awareness. Now moving into groundwork - involve patients and nurses.
10.2 Erik Gerritsen
Secretary General, Ministry of Health, Welfare and Sport of Netherlands
Featured patient, Tim Kroesbergen. Using online community forums for patient empowerment, and tele-health to reduce complex and time consuming travel barriers for him.
The use of GPS tracking for elders with Dementia allows some care organizations in the Netherlands to allow their clients to wander freely. This reduces chemicals, restraints, slows progression of the disease, and improves quality of life.
MedMij is a Dutch personal health record program standards to exchange data on HL7 FHIR. It allows patients to coordinate their electronic health records from different organizations. Currently early implementation.
10.3 Elizabeth Canis
VP Strategic Initiatives, Anthem
Local healthcare and local market dynamics matter.
700-800 minutes per year. A stat Elizabeth heard from a Kaiser physician a few years ago, about the amount of time the most chronically ill patients spend with their physicians per year. Not even 15 hours.
Claims data isn’t that useful for insights.
Consumers want to change their behaviour and be healthy.
Anthem
One of largest insurance payers in USA. Covers 1 in 8 Americans.
Focusing on: chronically ill, personalized patient insights (small and focused, rather than dramatic lifestyle changes), supporting caregivers,
How can we get people to care if they don’t have time, if they're aren’t able to get off work, if they can’t afford transportation?
Session 11
Digital Surgery
11.1 Shafi Ahmed
Professor of Surgery and Associate Dean, Barts Medical School
Digital health and digital medicine -> now it’s time to start talking about digital surgery.
2001 - transatlantic robot-assisted telesurgery". Using fiberoptics a surgeon in NYC removed the gall bladder of a woman in France.
AR in surgery is happening. FDA gave first approval in October 2018 to an AR solution for HoloLens.
How would you treat appendicitis in space?
Surgical outcomes data publicly available:
Mortality is a crude outcome, how do we create a ‘black box’ for the operating theatre to be able to go back and see where mistakes were made so that we can learn from them.
11.2 Carla Pugh
MD PhD Professor of Surgery Stanford
Current operative reports are verbally written. What does “inserted with ease” mean? What did the “extensive adhesions” look like?
Physician written reports are a nightmare to use if the goal is to be able to do operative outcome research. They are not standardized.
Proposal: Over the last 17 years, Carla has done simulations of over 30 different clinical scenarios with 18,000+ physician encounters and recorded the data from sensors:
First, she has physicians come into the simulation OR, and collect data from 100 different people doing the same operation. Now there is a fingerprint of what the haptic information is like.
Now you can collect objective data about different surgical skills. For instance, using this data Carla can comment that a trainee has trouble with depth perception.
The motion data can be compared with the ‘final product grade’ (eg. how well the final surgical site looks). And now the outcome can be predicted before hand simply based on motion data.
Actually, Carla can assess a surgeon’s quality of skill within the first five minutes of an operation, based on the movement data from the very first anchoring suture.
This haptic and sensor data will eventually form part of the medical record.
11.3 Jean Nehme
MD CEO and Co-Founder, Touch Surgery
Jean built initial version of Touch Surgery with his friend (they have since hired a talented team).
It takes surgeons and trainees step by step through an operation, and allows them to learn, test themselves, and rehearse procedures.
The tool was made available for free online, and has had a lot of uptake from both clinicians and patients.
They have spent time working to build a digital map for surgery - one that incorporates surgical cognitive tools - and alerts the user to risks and steps.
Currently deployed across 200 procedures. The App still is free.
Left side: can see difference between novice and expert. On right see learning curves
Randomized Control Trial of Skills Transfer: From Touch Surgery to Laparaosocpic Cholestectomy.
Randomized 40 people, to use the app or control (video and steps). Each then preformed a laproscopic cholecystectomy on a simulated model in the lab. They were assessed by a blinded evaluator. In the end the group that used Touch Surgery performed twice as well.
Saw same results from RCT for chest tube insertion.
Product is used worldwide in particular in low and middle income countries.
Currently in 160 US residency training programs. They provide data back to their program assessors and can then certify they understand the process.
This graph shows an expert surgeon using the App prior to a surgery.
Preparation tool: helping people learn how to prepare using actual patient details. Not just walk through an operation, but walk through the specific operation using a patient’s anatomy.
Real-time in surgery guidance system: using camera they are able to map the operation, know what the next steps are, and suggest them. This is good for new surgeons. For expert surgeons it is more helpful to provide advice on risks of particular steps. The scrub tech can see what tool to hand next.
Surgery global metrics [from slide]
$1 trillion USD spent on surgery in the US
11,300
11,4000 operations every hour in the US
322 surgical procedures per year performed worldwide
5 billion people without access to safe surgery
143 million procedures per year short of minimal standards
“Computers are incredibly fast, accurate and stupid. Human beings are incredibly slow, inaccurate and brilliant. Together they are powerful beyond imagination”
11.4 Stefano Bini
MD Professor of Orthopedics, UCSF
The adjacent possible: idea introduced by Steve Johnson in book Where good ideas come from (2011). Initially suggested by Stuart Kaufmann 2002 in evolutionary biology.
Suggests - ‘innovation usually happens in the realm of the adjacent possible’
Technological Adjacencies: easy to imagine the adjacent technologies available
Social Adjacencies: law, governance. These can slow innovation and limit the space
Alternate payment models (APM) transfer risk from the payer to the provider. Transfer is via Pay-for-Performance (P4P), Commercial Bundles, Accountable Care Orgs, Medicare Advantage, and Integrated Delivery Networks.
The problem is that providers have not had to deal with patient risk in the past.
This has created new opportunity on provider side to quantify patient risk. One of first areas for bundled payments was in orthopaedics.
eg. ClarifyHealth - able to stratify patient risk in orthopaedics around 200+ risk factors. Also able to quantify the value of different physicians based on their operating quality and costs.
Other mentions
Skilled based certification model.
3D printed implants.
Smart implants. have sensors inside them, so they can detect how an implant is doing. This is important, because if you can monitor a device you have better understanding if its performance, and then the provider can assume more of the financial risk.
Myo-electric prosthetics.
Exoskeletons
20% of cost in knee replacement is after leaving hospital. Virtual tools for physiotherapy to help understand what patients require it, and which don’t
eg. UC Health Colorado - implemented AI based scheduling tool, and resulted in 4% increase in revenue per year ($15 million), and released 47% more blocks.
eg. CloudMedx - Cognitive AI support. Gave modified medical board test. Residents got 68-81% writing test over 2.5 hours. The AI scored 85% writing it in 5 minutes. Resident with AI resulted in score of 91%
Mobile surgical suites
A robot connected to a medical student may be able to do an operation as well as the surgeon who designed the robot - helping solve access
Session 12
It's All About Timing: Health, Aging and Interfaces
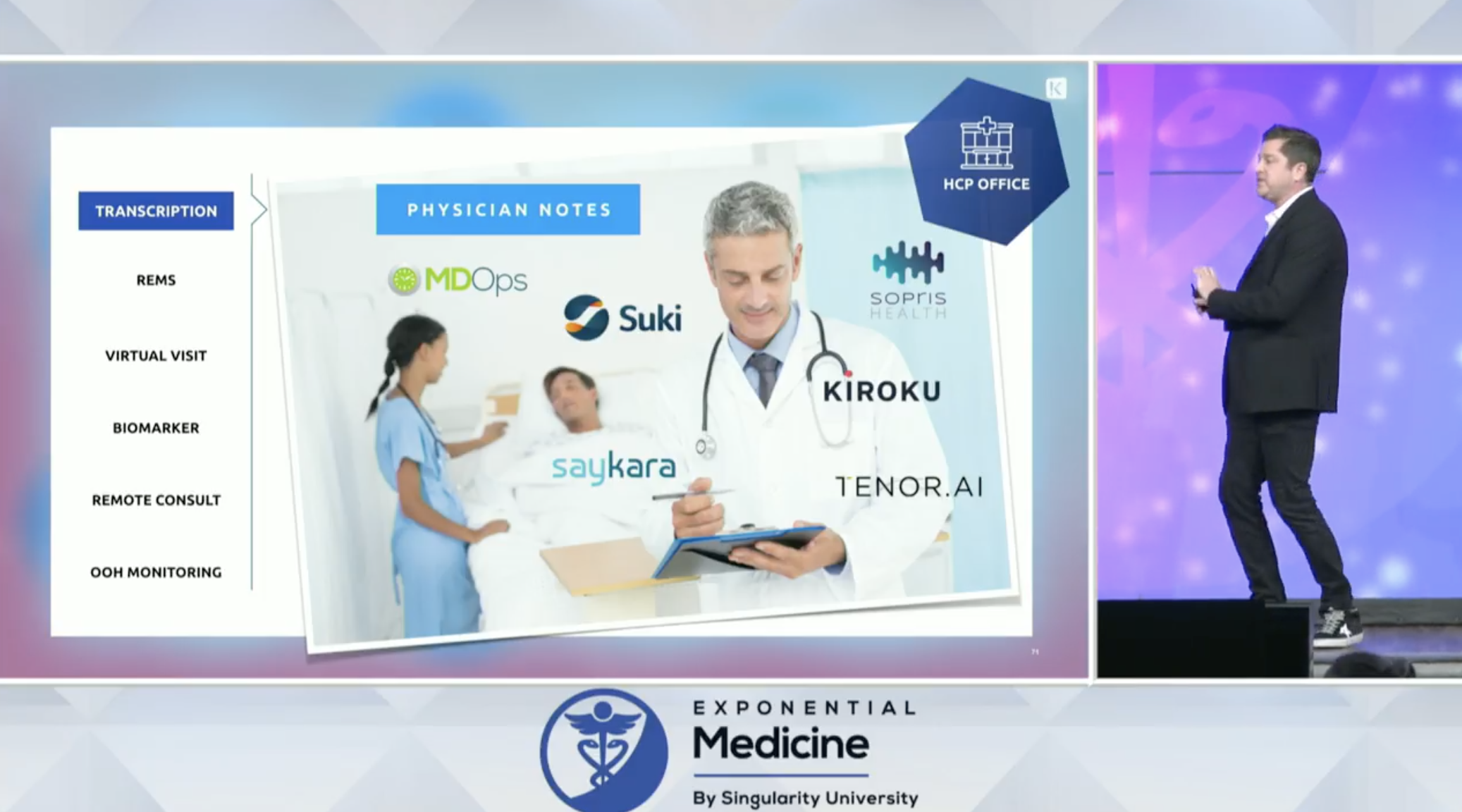
12.1 Leerom Segal
Co-Founder and CEO, Klick Health
More technology = more complexity —> —> complexity endangers lives in healthcare
Voice is the most natural tool in healthcare.
5 reasons voice is today’s battleground for big tech
1. Discovery - many of the biggest companies rely on discovery (eg. find something to buy, or to answer your question). Voice is the best way to do this.
2. Sound - there is a difference between voice and sound. Sound carries the meta-data about your surrounding. This is why black-box on airplanes is useful.
3. Convenience - the benefit of voice is even greater than benefit of touch screen interface. Requires less cognitive load
4. Intimate - voice and sound tells the story of your reality more than still images do.
5. Cloud - it’s easier to upgrade voice tools without need for new hardware.
Where will cultural norms end?
Initially there was resistant to CCTV cameras when they were introduced in airports and schools. Then the debate moved to body-cams on law enforcement. Cultural norms change over time.
If you always had a microphone recording you and room, it would know your preferences and needs much better.
US Coast Guard was having problems with hoax calls. So they used voice technology to tell difference between real vs drunk voice, and what the background sounds were (eg. actual ship vs someone’s basement).
Touch Screen Interface, why it took so long to occur
Why is voice taking off now?
Why is voice important - also its cheap relative to other customer technologies:
12.2 John Brownstein
PhD Chief Innovation Officer, Boston Children’s Hospital Professor, Harvard Medical School
Examples of voice in healthcare:
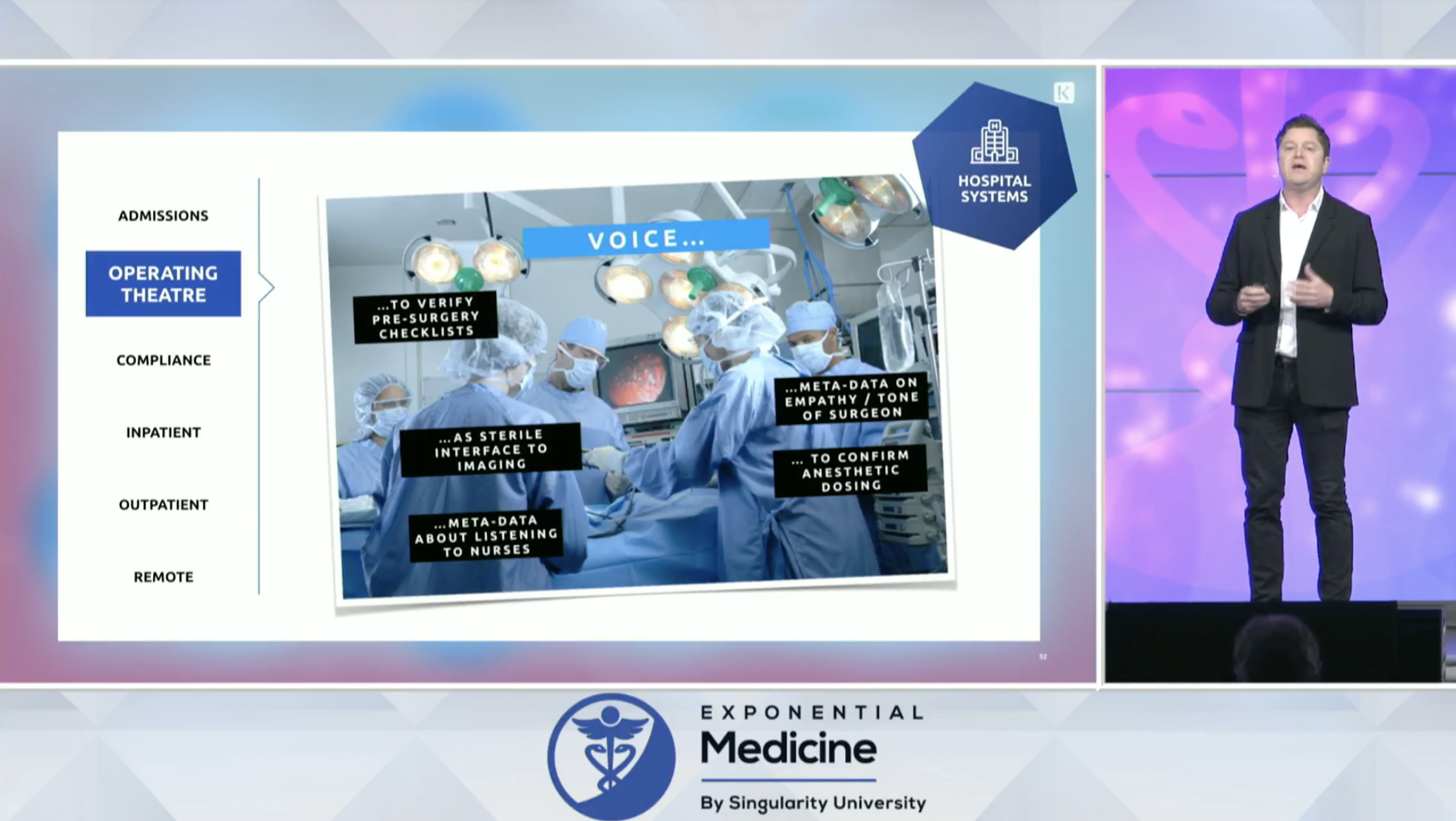
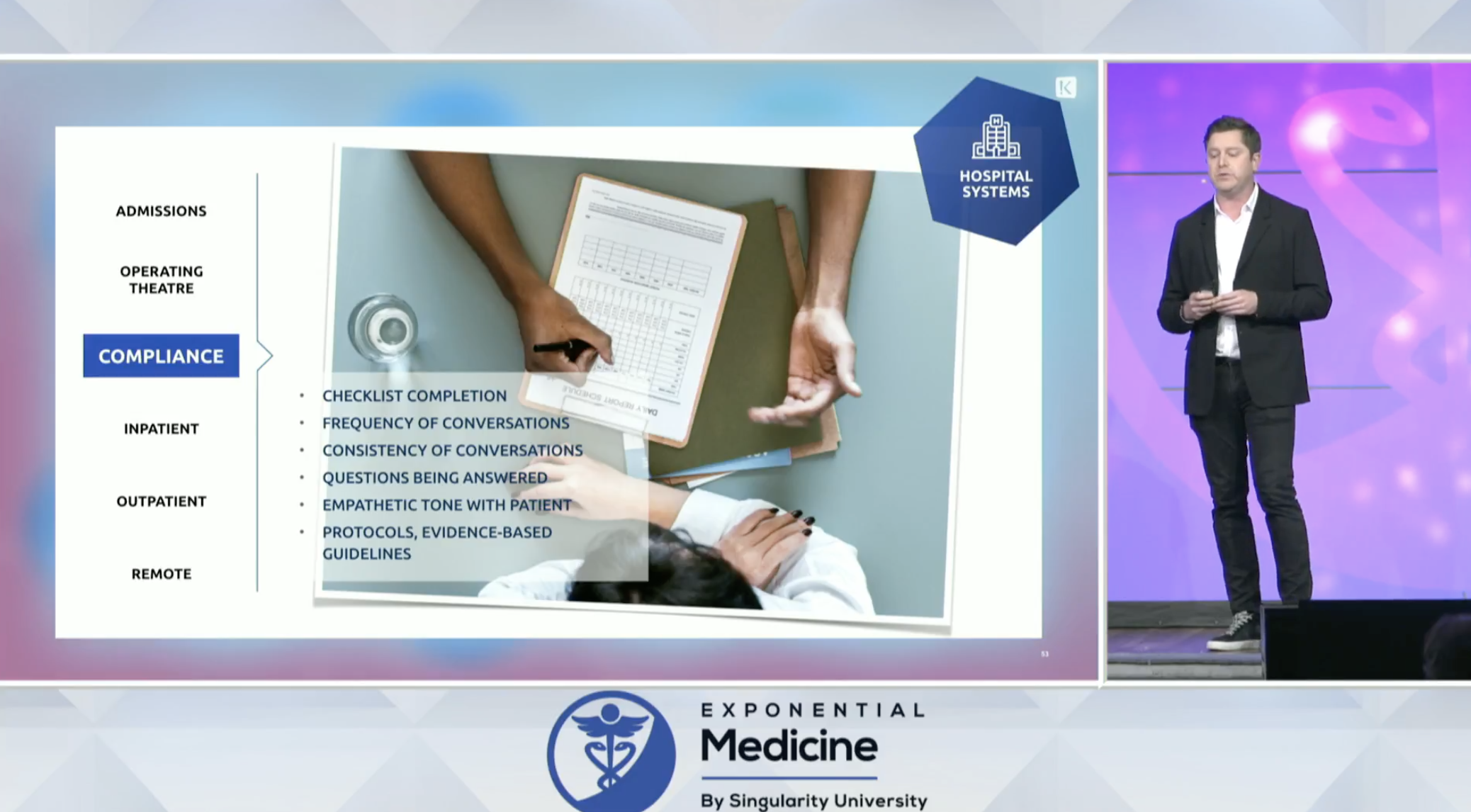
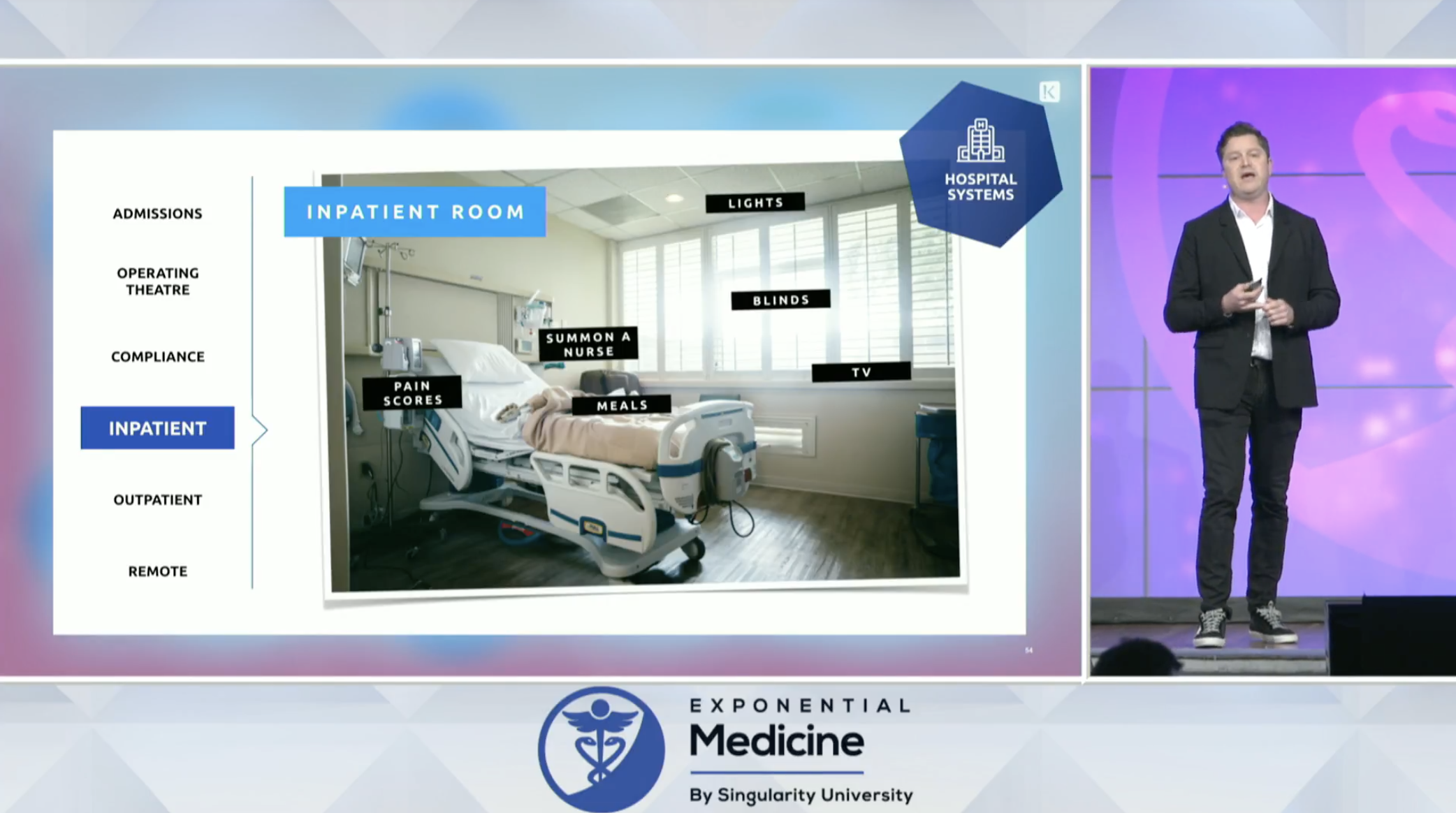


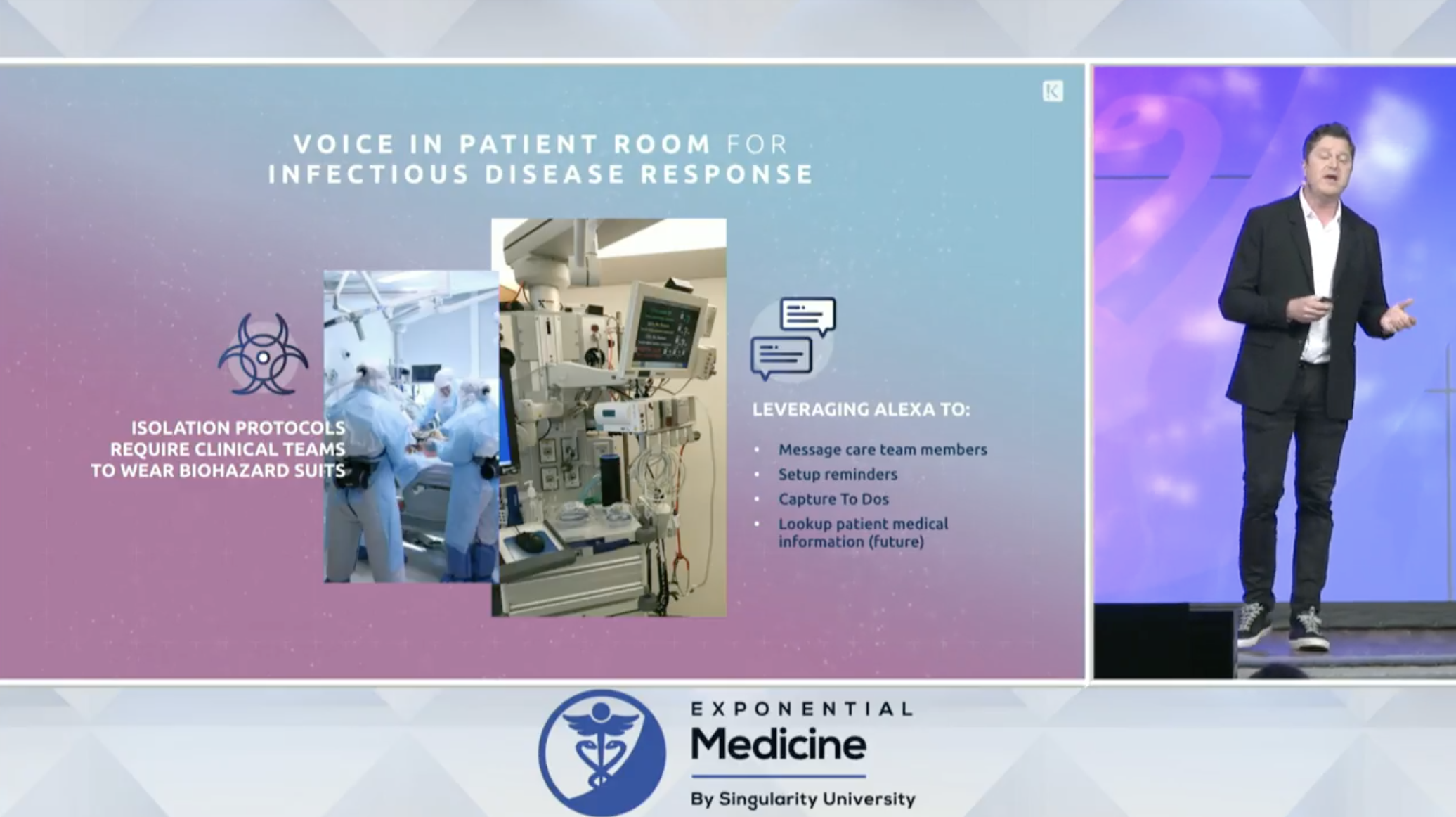
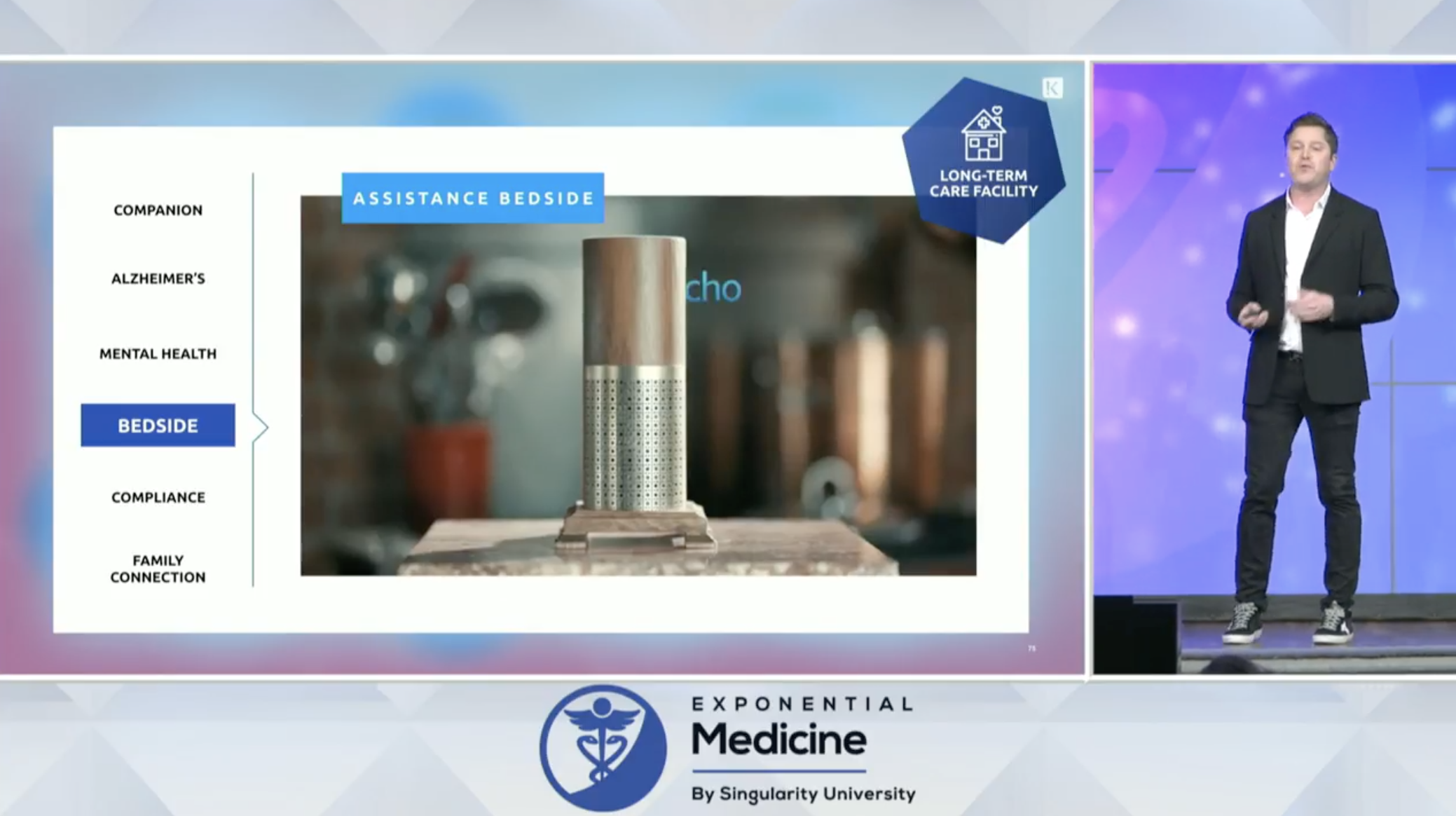


Boston Children’s has laid the groundwork for voice & is using in pilots in their ICU, as surgical checklists, and in the transplant organ verification process.
Concerns about voice:
Voice as a biomarker:
Voice will be closely linked into purchasing and consumer behavior
Voice as a right: loss of voice from diseases from ALS - how can tech give this back to people? Able to create a ‘voice bank’ - where you can spend 20 minutes reading a script and then the computer can generate sentences and use your voice to generate them.
“Human imagination is a preview to the future” - Albert Einstein
12.3 Satchidananda Panda
PhD Professor, Salk Institute for Biological Studies
“For every person they do help, the ten highest grossing drugs in teh United States (in 2015) fail to improve the conditions of between 3 and 24 people.” - Schork, NJ, 2015, Nature
Proposes that the variation in our natural circadian rhythms is connected to chronic disease.
Every cell in body has its own circadian rhythm and clock.
Melanopsin is a blue light sensing protein that influences this. Discovered 16 years ago.
The solution, is to help change the way light is designed and used.
The ‘blue light filter’ on phones, is a result of this work.
But. Light is not the only factor that influences circadian rhythms, food as well can over-ride these.
What happens when food is presented at the wrong time?
Experiment. Took two groups of mice, and the only variable they randomized them to was when they ate. One group could eat when they wanted, and the other group only for 8 hours a day. (note: the total amount of food was the same).
By the end of 18 weeks, one group of mice weighed 28% less, and this was the result of a 70% reduction in body fat.
They repeated the experiment changing different eating hour windows 8, 9, 10, 11, 12, hours, weekends off. Different diets were also tried, high carb, high fructose, high sucrose, high fat. Again - same total daily calories.
The results were the same, those mice that ate within a 8-12 hour window did the best. When mice that were sick were placed on a 8-10 hour eating window, it reversed disease.
Appears timing is more powerful than calories.
Did experiment creating online website, mycircadianclock.org. People tracked on an app when they ate.
People who don’t do shift work, 50% of them eat for 15 hours or longer a day including first foot / to last.
Asked people to eat everything within 10 hours.
Over 10-12 weeks, people had benefits of sleep, weight, heart, and cancer risk.
The timing of surgery, flu shot, and chemotherapy can have almost 20% impact on long term outcome.
Book: The Circadian Code
12.4 Jeffery Bleich
Founder and CEO Pulson
How can we make exercise easier for everyone?
Counter-pace technology. Have you ever wondered why sometimes when exercising sometimes it feels great, and other times it feels very hard?
The health benefits of exercise
Note: the musculoskeletal system - is a pump - to go with the pump of the heart.
The best runners in the world step at their heart rate, because they are stepping during cardiac diastole, and this is adding to the musculoskeletal pump effect.
We have known that medical counter-pulsation machines (large loud machines that do this), have heart and brain health benefits such as increased cardiac collaterals.
Jeffry’s company, Pulson, has created an App that connects to a cardiac heart rate monitor to assist so they can help you coordinate these cycles.
The same paced counterpulsation could be used to sync pacemakers in those with congestive heart failure.
Data from using US athletes running:
When the pace matches the diastole of the heart rate there are dramatic improvements in hemodynamics - such as decreased blood pressure and reduced heart rate.
About half of professional athletes naturally step in sync.
Though not as many college athletes do. Training college athletes to run in sync can improve 6K split times by ~3%
Brain blood flow increases.
Multiple studies looking at counterpace vs placebo RCT
12.5 Julia Vishnepolsky
MA LMHC R-DMT Expressive Arts and Dance Movement Therapist, Adult Day Health Care
Alma - Program taking high school students and changing their perception of aging by having them interact with those in nursing homes.
Goal to help reduce isolation in the elderly
Session 13
Curing the Incurable
Jack Kreindler MD
Founder & Director, The Centre for Health and Human Performance
Parker Moss
Health Technology Entrepreneur in Residence, F-Prime and Eight Roads
Book: Man’s Search For Meaning
One thing that can never been taken away, is how we respond to circumstances.
Things we need to be doing:
1. Learning from our data.
2. Cancer more of a chest game, how can we plan for multiple steps
3. Adaptive trials (not just randomized control trials)
Session 14
Connecting the Dots: Solutions at Scale
Rasu Shrestha MD MBA Chief Innovation Officer, UPMC Executive Vice President, UPMC Enterprises
Move from patient centred care -> to person centred care.
Everybody loves to innovate, but nobody likes change.
We are at strategic inflection point. Though, in healthcare it seems like nobody is in a hurry.
Because UPMC is both payer and provider, there is focus to keep people well. To use the hospital as a ‘control center’ to keep patients out of it.
For instance, before heart failure patients are discharged, they are risk stratified, and those who are high risk are sent home with monitoring equipment.
A blind spot we have, is why do patients opt out of interventions?
“Not just adding year to life. But adding life to year.“
“Surviving to thriving”
“Innovation done right makes technology invisible”
You may be interested in the Notes from Day 1, Notes from Day 3, or Notes from Day 4.
All slides are from the Singularity University’s Exponential Medicine Conference YouTube live stream November 5, 2018.
Watch past Singularity University videos on their channel.
To register for next year’s conference, please visit their website, https://exponential.singularityu.org/medicine/ It sells outs, so register early.






