Exponential Medicine, Day 3 - Cool Stuff Summary (Nov 6 2018)
This is a collection of the cool ideas and my personal notes taken from Day 3’s presentations.
I wasn’t able to attend Exponential Medicine this year, but enjoyed watching the live stream from Kenya.
You may be interested in the Notes from Day 1, or Notes from Day 2, or Notes from Day 4.
Watch video summary of this post, or search on your podcast app: Gregory Schmidt
Day Three
Tuesday, November 6th
Session 15: Exponential Organizations
Salim Ismail Author, Exponential Organizations, Chairman, ExO Works, Board Member, XPRIZE, Global Ambassador, Singularity University
Session 16: NeuroMedicine at the Frontier
16.1 Divya Chander MD PhD Neuroscience Chair, Singularity University
16.2 Matteo Lai CEO & Co-Founder, Empatica
16.3 Ariel Garten & Graeme Moffet Co-Founder, Muse
16.4 Mary Lou Jepsen PhD CEO & Founder, OpenWater
16.5 Eric C. Leuthardt MD Neurosurgeon, Director of the Center for Innovation in Neuroscience and Technology, Washington University in St. Louis
Session 17: (im)Patient Innovators
17.1 Godfrey Nazareth President & CEO, X-Biomedical, Inc.
17.2 Mette Dyhrberg Founder & CEO, MyMee
17.3 Mariya Filipova Chief Innovation Officer, Anthem
Session 18: Future of Work & Investing
18.1 Vinod Khosla Founder, Khosla Ventures
18.2 William Morris MD Associate Chief Information Officer, Cleveland Clinic
Jennifer Radin, Deloitte
Shawna Butler RN MBA Nurse Economist and EntrepreNURSE-in-Residence at Radboud University Medical Center
Session 19: Care Reimagined; Connected, Digital and Virtualized
19.1 Jay Parkinson MD Founder & CEO, Sherpaa
19.2 Lara Jana MD Pediatrician, Associate Professor, Penn State
19.3 Walter Greenleaf AR & VR Thought Leader
19.4 Justin Barad MD Founder & CEO, OssoVR
Session 20: Radical Interoperability
John Mattison MD Chief Medical Information Officer, Kaiser Permanente
John Nebeker MD MS Deputy CMIO, Veterans Health Administration
Shannon Sartin Executive Director, Digital Services, U.S. Department of Health and Human Services
Session 21: Lessons in Leadership
Jason Tuschen & Jason Torey Former Navy SEALs, Randori Tech
Session 22: Reshaping Pharma, Discovery & Trials
22.1 Noah Craft MD PhD CEO & Founder, Science 37
22.2 Mei Mei Hu CEO & Co-Founder, United Neuroscience
22.3 Onno Faber Founder, RDMD
MEDy Awards
Session 15: Exponential Organizations
Salim Ismail Author, Exponential Organizations, Chairman, ExO Works, Board Member, XPRIZE, Global Ambassador, Singularity University
X Prize Board of Trustees & Benefactors
Clean water extraction prize just awarded: Can you extract 2000 litres from atmosphere per day using renewable energy for cost of less than 2 cents a litre?
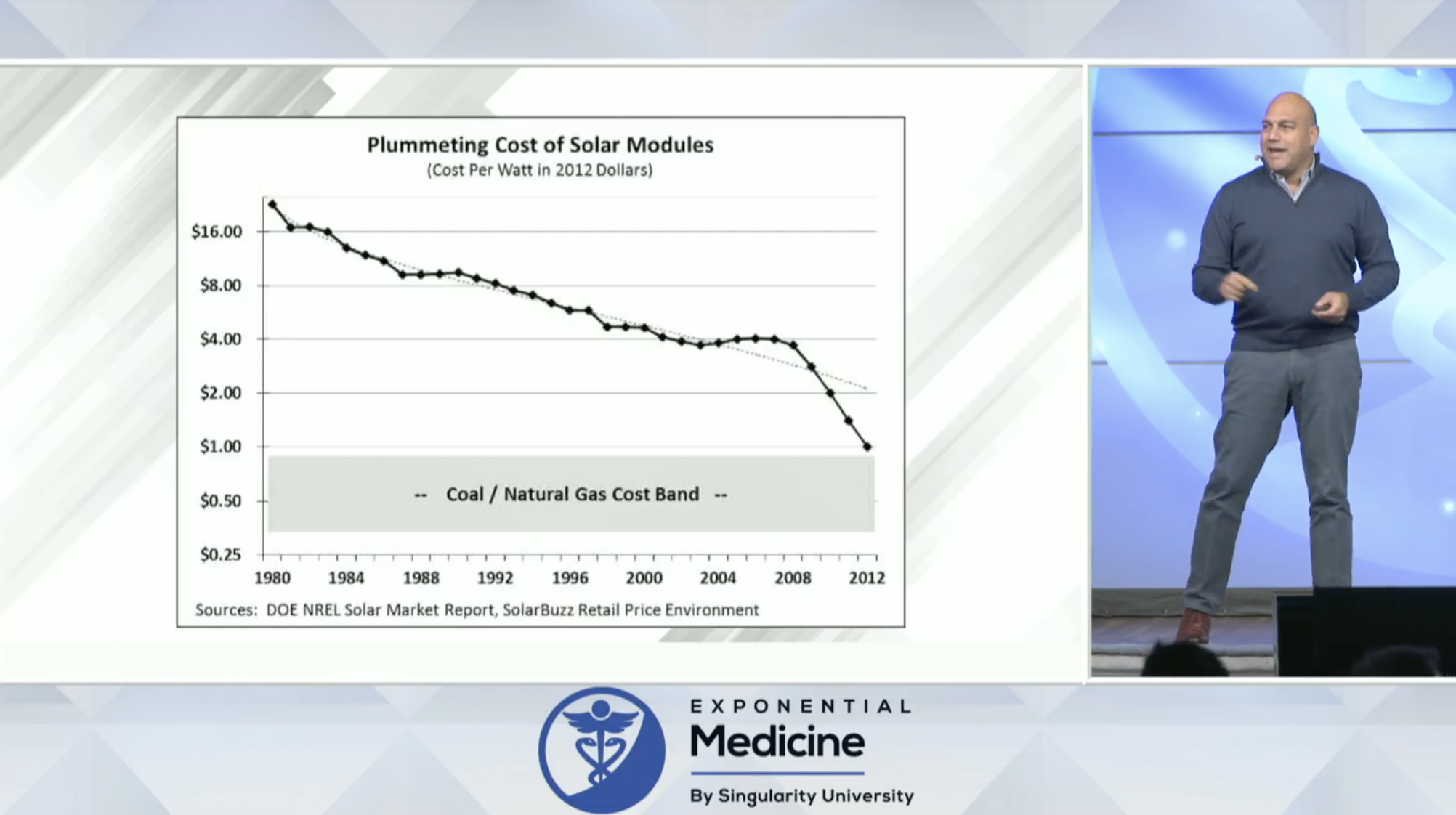
700 year graph of the cost of light. Same cost curve with gene sequencing. Same with cost of solar energy.
Salim experienced this effect of Moores Law at a macro level, in the improvement in the self driving functionality of his car within 18 months.
We use a ‘push model’ for education. We need to move to a ‘pull mode’.
Institutional challenges around the world:
‘Metabolism of economy is increased’ - it used to take 20 years to create a billion dollar marketplace, now that can happen in months.
Examples of industries that had major deflationary effect when technology was brought to them.
Reduced costs in some areas, will lead to more discretionary funding to use in other areas.
eg. Electrician was going to charge $2500 to install lightbulb in his backyard. Instead on Amazon found solar powered, motion controlled light for $9.99. He bought four of them.
We have trouble spotting doubling patterns when they are really small.
We think technologies are ‘black swans’ (came out of nowhere), when in fact they are exponential (just that the doubling effect for many years is hard to see until it reaches the kick of the curve).
eg. Most people have heard of 3D printing within the last 5 years. A few maybe heard of it 10 years ago. Though in fact the technology is over 35 years old.
eg. Drone technology is doubling every 9 months in cost/price performance.
eg. Cost of sensors for a driverless cars a decade ago was $200,000 a car. Now its under $1000 a care.
eg. Lidar cost $75,000 in 2012, in 2017 it is $50. Part of the reason for the drop is, multiple technologies within the device are all undergoing exponential cost decreases, and this creates an aggregate multiplier effect.
eg. of the growth of solar energy. The black vertical line is the actual growth of solar energy. The horizontal colored lines are the ‘expert predictions’ of where solar energy will go. The human predictions are always linear. Same trend was seen in cellular phone predictions.
Sequence of what happens after a domain is digitized:
“Any company designed for success in the 20th century is doomed to failure in the 21st” - David Rose
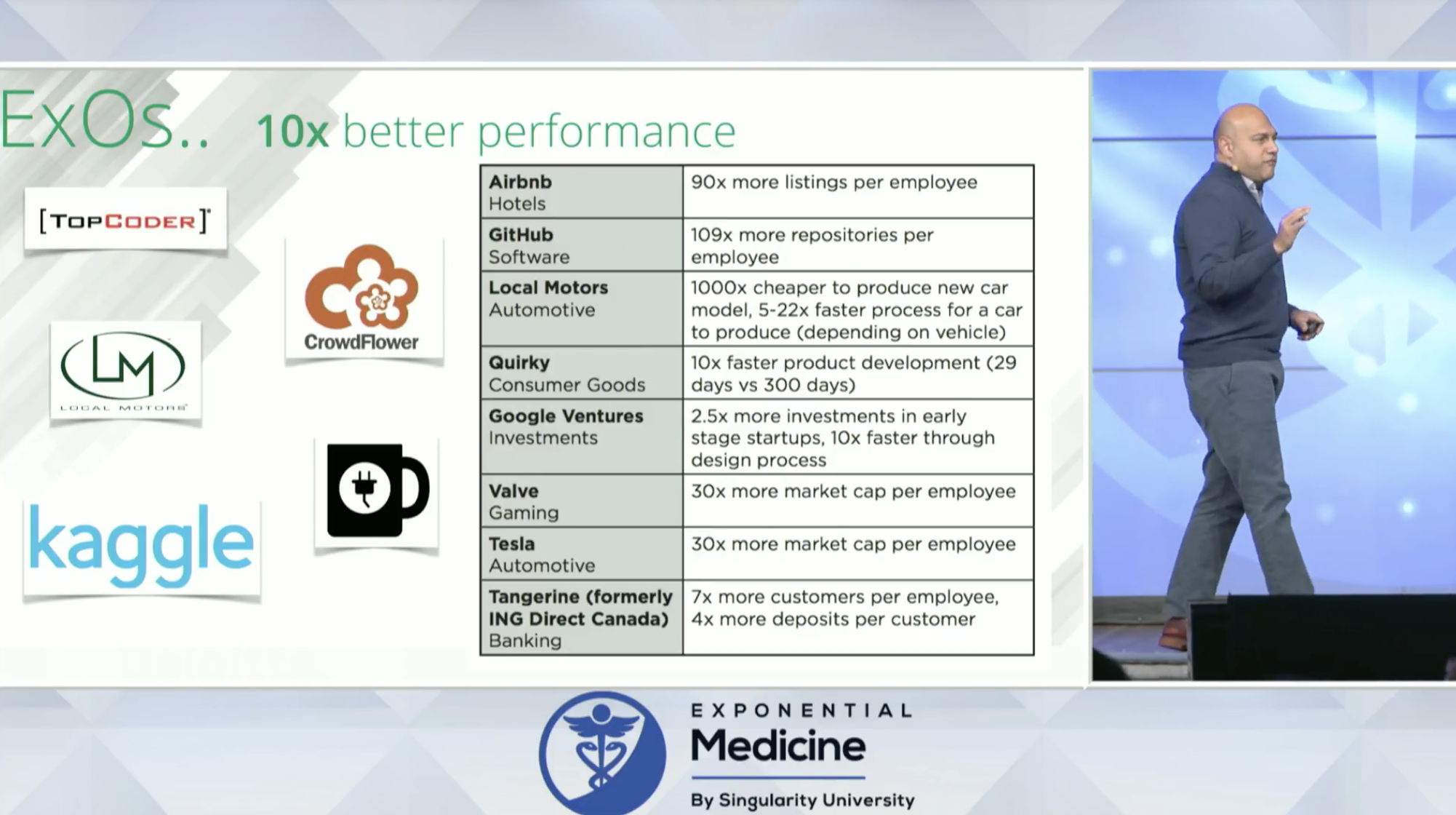
eg, of how new organizations deliver more than 10x performance over prior companies in the same space.
Medium Post: The Secrets of Unicorn Companies: And the 100 Most Scalable Organizations
ExOs - Exponential Organizations - Website, with list of the top 100.
The highest ExO they ever found was Github - Microsoft paid $7.5 billion for a company that has no workforce, not intellectual property, no assets.
Exo is based on 11 characteristics, most important is that are centered around a ‘MTP’ Massive Transformative Purpose. Adding at least 4 of these to your organization dramatically increases its efficiency.
Standard business is balance of demand and supply. The Internet dropped the cost of demand (eg. acquiring customers) dramatically. Now companies are able to also drop the cost of supply (eg. adding another property to AirBnB).
The Fortune 500 companies were ranked using ExQ scores:
The stock market performance correlated to ExQ scores too:
Investment in the top ExQ organizations would have resulted in 3x stock market performance over the S&P.
“Do not do disruptive innovation inside the mother ship”
“The [company’s] immune system response is too powerful”
This is in part why Google has separate companies to do this. This is how Apple innovates, by taking a a team of engineers and putting them on a secrete project. [Amazon also does this very well]. “Do not try to innovate in the main organization and push it out”
eg. of traditional companies trying this: Ikea building vertical farming, Corona beer moving into weed, Nestlé creating personalized diets in Japan based on people’s DNA
The ideas created outside the organization likely won’t be able to be brought back into the organization, but may benefit better by being spun off as a separate / side company. Bringing in something exponential to an existing linear organization may catabolize the innovation.
Salim runs this as a 10 week program for companies. They have two streams, one works on EXO ideas on the edge of their organization, and another group focuses on how they can transform the current internal organization using EXO ideas. That way the new incumbents working on the external ideas, will not be attacked when they come back to the main organization.
This process is available as a book: Exponential Transformation: The ExO Sprint Playbook to Evolve Your Organization to Navigate Industry Disruption and Change the World for the Better [amazon] [book website]
This has been done in both private sector, and now public sector (Via Fast Track Institute).
4 Observations About World
1. 20 Gutenberg moments are coming (AI, solar, blockchain, CRISPR, neuroscience, etc)
2. It is breaking all our institutions
3. Current leadership doesn’t know how to think exponentially
4. Most of impact is happening not at city level, but over small regions.
Session 16
NeuroMedicine at the Frontier
16.1 Divya Chander
MD PhD Neuroscience Chair, Singularity University
Divya went into anesthesia because her interest in neuroscience made her interested in how we can manipulate and study human consciousness.
READING BRAINS
You can track loss of consciousness, ‘sweet spot’ for anesthesia, and then best way to bring patient’s back from anesthesia.
Stanford: combining databases from Sleep lab (750+), Anesthesia (730+), and Epilepsy (136,000+). Then mine them for biomarkers.
Also creating a ‘drug dictionary’ of what every drug looks like on EEG.
WRITING BRAINS
Common technique is deep brain stimulation. Electrodes placed into brain while a patient is awake. In this example the tremor disappears from the patient while playing their violin. Technology is not perfect.
New field for writing brains / deep brain simulation is called, “optogenetics”. Much more specific. (1) DNA is taken from microbes that are sensitive to light. (2) This DNA is injected into specific neurons (3) Now neurons can be activated by light. …but still invasive, requires a fibre optic implant.
Newest techniques (non-invasive ie. no whole in brain required).
eg. mechanotrasduction - pressure receptor. Experiment placed these channels into the brain of a roundworm. Then low-pressure ultrasound was able to change the movement of the worm.
eg. Nanoparticles that take in infrared light, convert it to blue light, and then these can be used to modulate neurons
eg. Leigh Hochberg - have grid of implants that sit on a patient’s motor cortex, that allows patients to control robots using just their thoughts. Newest work is to implant a ray of electrodes into a patient’s somatosensory cortex, so they can actually feel the sensation of the robotic arm. This is invasive (required implant, and then connection into the brain).
Research in Australia, to connect these interfaces an intra-vascular bundle (rather than a hole in the skull).
Another way is use of a piezocrystal, that can be activated with external energy as a mechanism to stimulate nerves.
New ways to non-invasively modulate the brain:
Focused Ultrasound
tDCS - Transcranial Direct Current Stimulation
TMS: Transcranial Magnetic Stimulation
Radio-energy
eg. of it in use:
Transcranial Magnetic Stimulation has been FDA approved for treatment of depression.
INSIGHTEC has FDA approval to start clinical studies to try and treat the amyloid plaques that cause Alzheimer’s disease.
Use of flashing lights and pink noise heard by ears to try and stimulate brain in ways that reduce amyloid plaques and improve memory to reduce Alzheimer’s (28 Feb 2018 Nature). Also work for Parkinson’s disease, and Migraine Headaches.
Papers in last five years showing noninvasive external brain simulation can improve working memory. And these studies are long lasting for at least up to 6 months.
Also being used now to improve sports performance.
First telepathy experiment in 2014. Sent thoughts
Now (Sept 2018) 3 brains connected together:
16.2 Matteo Lai
CEO & Co-Founder, Empatica
Created a product initially for autism, and then a patient has a seizure. The sensor they were wearing at the time went off chart, and based on this they started working on a device for epilepsy.
Embrace - first smart watch to be cleared by FDA. Uses machine learning to detect epilepsy events, notify patients and families.
Eleven months worth of data - it identified an epileptic event almost weekly.
It tries to look at factors influencing a patient’s seizures and how they can reduce this.
Example of study that took patients who were resistant to drug therapy for epilepsy, and treated them with biofeedback. It worked.
Companies doing digital therapeutics in this area: Empatica, Akili, Pear Therapeutics, Headspace.
16.3 Ariel Garten & Graeme Moffet
Co-Founder, Muse
Neurotechnology - is all over the mainstream news, and we know what the end goal is with regards to seamless human/machine interfaces. But, what technology is ready today for market?
Original Wearable Computing Group, ad MIT Media Lab - 1993
EyeTAP vs2.0 2001 - goal to control interfaces without use of hands.
In order to use this technology to control computers using your mind, you had to learn how to clear your mind. So….a meditation tool was created.
Benefits of Meditation
Over time meditation changes the anatomic structure of the brain.
As one ages their ‘actual age’ grows faster than their ‘brain-age’ - meaning the brain has less atrophy. The brains of meditators 50 years old, appear 7.5 years younger than non-meditators.
Within four weeks we see difference in the brains of meditators when evaluating perceived stress via EEG. We also see neuroplasticity in the area of executive control functions within four weeks of meditation.
Discovering new EEG patterns from large scale EEG data.
MUSE 2.0
16.4 Mary Lou Jepsen
PhD CEO & Founder, OpenWater
She has worked in Asia extensively in manufacturing and shipping digital products. Previously ran advanced AR/VR at Oculus and Facebook.
Her goal is to be able to replace a giant MRI machine, with a wearable. Yes, this does sound impossible.
They imagine the cost of the device being the same as a cell phone, and the cost of a scan the same as a phone call.
How
Infrared light hoes through body.
The problem is the light when it gets to the other side/surface is scattered, but this is solved with processes developed in the field of holography (aka Holograms)
Ultrasonic Scanning can be used to focus the light and sound.
This summer: able to image tissue at 0.5mm resolution. Slightly higher than standard MRI
Blood - is very easy to see using this technique. This is helpful because cancers undergo angiogenesis and increase blood flow, and cardiovascular disease reduces blood flow.
To detect if blood is fresh vs old they can use two different wavelengths of light.
Wanted to see if they could get to same resolution of fMRI (millimetre x millimetre). Yes, they can do this.
Wanted to see how far they co go - and got down to a few microns resolution. That benefit is not
just 1000x better, but because it is 3D (1000x1000x1000) it is actually a billion times better resolution.
Lab prototype from last spring 2018
Openwater has developed new components in: camera chips, ultrasonic chips, and lasers.
Within last few months they have made improvements in:
10x less light needed
100x image quality increase
100x smaller footprint
100x faster scan speed
Where is this going?
a) 2/3 of global population doesn’t have access to imaging tools
b) Most imaging tools are still too expensive even for those with access - for instance, no country uses MRI as first modality for general breast cancer screening, even though it is better than mammography.
c) reading brains….which we can already do…it is just a resolution problem (and lack of data problem).
In 2011 scientists played Hollywood movie trailers to people in an fMRI machine to map how their brain responded to the images. They then were able to reconstruct from fMRI brain activity what people were watching.
Similar, another group in Japan recorded fMRI of people sleeping, and would ask when they wake what they were dreaming about.
The accuracy of it is getting better…
The bet, and value of a cheap, portable, wearable tool….
These types of tools will be of tremendous use when combined with focused ultrasound. This chart shows the state of focused ultrasound - and it is exploding.
16.5 Eric C. Leuthardt
MD Neurosurgeon, Director of the Center for Innovation in Neuroscience and Technology, Washington University in St. Louis
How we can connect better to our minds, to heal during stroke.
“How do you fix a broken brain? You can’t place stitches on it, or a band aid, or a cast.
You realign it in Time”
Brian Computer Interface: Sensors / Computation / Output
Brain computer interfaces used in people with limb and spinal injuries. But the classic thinking was that it could not be used for those with stroke, because that part of the brain no longer functioned.
Creation of a brain computer interface for patients after stroke.
Hebbian Learning - related to the synaptic strengthening of neurons. The uninjured part of the brain can learn. It retains the intention to move the hand, but lacks the ability to execute hand movement because that part of brain was injured with stroke.
The brain computer interface can trigger a robot on the patient’s hand to move when they intend it to move. This movement brings signals back to the brain that the hand moved.
The goal, is that a stroke patient can use a IpsiHand System for several weeks to train the preserved part of the brain to not only intend to move the hand, but develop the ability to execute hand movement, and therefore not even require the brain computer interface or robotic hand in the long run.
Their finding showed benefit in 70% of patients. It was featured on cover of stroke. And it doesn’t require a surgery or medication.
Rick started to even be able to regain some of his ADLs that he had lost years prior.
How can we heal the brain when it develops depression?
Clinical depression creates dominance of default mode network.
A new approach: vagal nerve stimulation is used to increase the brain’s plasticity, and digital therapeutics are used to re-shape the brain patterns.
To access the vagus nerve, the easiest external way is via the trans auricular branch which can be stimulated via the ear.
There are multiple ways to shape the mind depending on the mental health condition. For depression, cognitive behavioural therapy is powerful. For PTSD exposure therapy using virtual reality helps.
Combining these ways to re-shape the mind, with vagal nerve stimulation to increase brain plasticity you can have better outcomes, faster.
Where is this going? PONG Moments
If you tried to explain to someone in 1972 where PONG would end up thirty years later (2002), with 3D console games they wouldn’t believe it.
And then if you showed the person in 2002 virtual reality, they wouldn’t believe it.
2004 was first time someone controlled a device using invasive cortical physiology (their brain).
2011 patient could now control a robot to shake a hand.
eg. Pong moment today: an electrode placed into temporal lobe enhances memory.
eg. Pong moment today: ability to share information between brains (ie. able to encode and decode information).
eg. Pong moment today: ability to ‘download’ memories. (ie. save encoded information to download later). Paper from 2013.
At the Center for Innovation in Neuroscience and Technology he runs they routinely hold “Invention Sessions”. where they bring in people who routinely don’t get together, and discuss both the problems and what is new in the field of neurotechnology.
Session 17
(im)Patient Innovators
17.1 Godfrey Nazareth
President & CEO, X-Biomedical, Inc.
Diagnosed with ALS (around same age as Stephen Hawkins).
If you can find what you are passionate about enough to die for, you can turn it into a cause to live for.
17.2 Mette Dyhrberg
Founder & CEO, MyMee
Autoimmune diseases - many different medical conditions - but why does it happen?
Using data analytics to try and understand what is triggering the immune system to fire against itself.
Multiple small case studies of patients with multiple auto-immune conditions, that can be reversed by identifying the non-obvious triggers that are setting off a patient’s auto-immune system.
17.3 Mariya Filipova
Chief Innovation Officer, Anthem
The problem with the Kubler-Ross Change Curve that all patients with a major diagnosis go through, is that it nadirs at depression. Mariya didn’t like that, so she changed it.
The curious mind is an excellent antidote to fear.
‘Surgery with sparing of the kidney….it can’t be done’
Personal story of how after presenting at Exponential Medicine help from around the world came in with suggestions on how to remove her very large tumour (Birthda). This year it was embolized. And then surgically removed.
Session 18
Future of Work & Investing
18.1 Vinod Khosla
Founder, Khosla Ventures
Most of the text in the summary is written directly from his slides…
“I gave a version of this talk three years ago, and not a lot has changed, except things are more certain and accelerating faster.”
Medicine does get better every decade. But it is making incremental progress. Not exponential.
PART 1:
The Problem: State of Medicine Today
1. 50% of MDs are below average (median).
“A physician actually got up and challenged me during one of my talks on this statement. That’s your below median physician”
source: math
2. 40,000+ patients in US ICUs may die from a misdiagnosis annually
Diagnostic errors in the intensive care unit: a systematic review of autopsy studies
https://qualitysafety.bmj.com/content/21/11/894
3. Doctors are surprisingly bad at reading lab results.
Washington Post Article Oct 2018
4. Human doctors: cognitive limitations, cognitive biases,
The Importance of Cognitive Errors in Diagnosis and Strategies to Minimize Them
http://www.jround.co.uk/error/reading/crosskerry1.pdf
Heuristic reasoning and cognitive biases: Are they hindrances to judgments and decision making in orthodontics?
http://www.ncbi.nlm.nih.gov/pubmed/21392683
Diagnostic error in internal medicine.
http://www.ncbi.nlm.nih.gov/pubmed/16009864
Reducing Racial Bias Among Health Care Providers: Lessons from Social-Cognitive Psychology
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2219858/
Teaching about how doctors think: a longitudinal curriculum in cognitive bias and diagnostic error for residents
http://qualitysafety.bmj.com/content/22/12/1044.abstract
Cognitive biases in medicine
http://evimedgroup.blogspot.com/2010/10/cognitive-biases-in-medicine.html
5. 100 cases of diagnostic error involving internists…cognitive factors in 74%.
(This can be eliminated. Premature closure was the most common cause).
Diagnostic Error in Internal Medicine. Mark L. Graber, 2005. JAMA
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/486642
6. In many records of high-risk diagnosis, high-information clinical findings were present and ignored
Presence of key findings in the medical record prior to a documented high-risk diagnosis. JAMIA 2012.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3384101/
7. The AHA/ACC made 7,196 recommendations…19% of recommendations of Class I Guidlines have Level A evidence….48% have Level C evidence (the worst kind)
Scientific Evidence Underlying the ACC/AHA Clinical Practice Guidelines. JAMA 2009.
http://jama.jamanetwork.com/article.aspx?articleid=183453
8. 40-50% of the recommendations made in guidelines are based on expert opinion, case studies, or standards of care rather than on more systematic trials and studies
American College of Obstetricians and Gynecologists practice bulletins: An overview 2006
http://www.ajog.org/article/S0002-9378%2806%2900300-0/
9. “One of my big beefs with medicine today, is that the treatment you get is based on the physician you get, not on the disease or problem you have” [I agree 100% this this. This is a huge problem, and major source of embarrassment to the field of medicine].
These were the individual results of an expert panel, asked to estimate the chance of an outcome based on an important procedure. They actually made a decision based on this…
The Challenge. JAMA 1990.
http://jama.jamanetwork.com/article.aspx?articleid=380215
PART 2:
THE SHIFT vs 1 - vss8
Moving from the practice of medicine -> to the science of medicine.
“Almost nothing (most) of what med school students are learning today will be irrelevant to the science of medicine in 15-20 years. Maybe 25”
“Machines will be better at integrative medicine.”
”machines will…learn across many good doctors, all research, all data, and get better rapidly with time starting as ‘bionic assistants to humans’.
The average patient will not be getting a median physician. They will get the best”
we’ll start with clumsy point innovations..
“Timelines are impossible to predict.” The important part is the generations of medicine
“In the interm, we will have upscaling of professionals. When I say 80% of what doctors do, people get upset. When I say nurses get upscaled to do more than a primary care physician, people get happy”
‘Technology will also upskill all medical professionals (nurses, technicians) and consumers…leading to a complete shift to how we mange care
Innovation Axes
Al 24/7 "almost free" physicians...
data driven personalized care: 30k not 30 longitudinal biomarkers
"omics medicine" & imaging replacing symptom based medicine
new tools: CRISPR, DNA/RNA, microbiome
Al based Imaging, image diagnosis, enhancement, new imaging modalities
Al enhancement for tools (imaging, drug discovery, diagnosis, surgical robots...)
Accessibility, immediacy, affordability... the great equalizer
CRISPR organs, 3D printed organs/parts, microrobots
The Shift: vs 1
Radiology: We are seeing it in radiology. Some algorithms are better than the average radiologist.
Seven years ago people laughed when I wrote my blog article in TechCrunch: Do We Need Doctors Or Algorithms?
“I reread it, and there is nothing I want to change.
This was implausible. And now it’s broadly accepted as it is happening.
Statins: Kaiser discovered using new statin protocols for in-hospital stroke patients reduced the death rate by 40%. This improvement is simply with a change in their protocol..
Results of the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial by stroke subtypes.
https://www.ncbi.nlm.nih.gov/pubmed/19228842
Google AI
Other predictions
“I think most conversations between patients and doctors will happen with an AI first for the next 10-15 years.”
“The quality of the triage function is almost more important than anything else”
Microbiome - being used to predict someone will have type 1 diabetes.
“diabetes will go the way of dropsy” Dr Dennis Ausiello
“The data science will differentiate the diseases not based on the symptoms, but on the causes”
Mental Health. Same thing.
Everyone will have an AI health kit at home, and nurse available ‘Doordash Style”
In 10-15 years, bionic assistants will be able to do 80% of almost every major speciality in medicine
Primary care to become most important part of medicine
Data to provide new insights. eg. to track Alzheimer’s.
Lab on a chip, at your home, 1000s of biomarkers…will lead to completely new forms of diagnosis
Large-scale holistic studies (see Lee Hood)
‘Network Medicine’
Drug discovery
More healthcare than sickcare
Goal: within next 10-15 years every human has access to primary level care through an AI physician. I think is possible.
Shift vs 5
Imaging, testing, diagnostics primarily handled by
algorithm. Consumer will have 24/7 specialty care.
Speculation: in the next 15-25 years
…data science will do more for medicine than all biological sciences combined
…and traditional healthcare will keep improving ALSO
“Humans matter on the human element of care.
I’d go look at UCSF film school. Because they have the most mirror mirror neurons”
Let’s not confuse “new medicine” with “better” traditional healthcare.
The innovation will come from outside the traditional healthcare system.
“I can’t think of an example within the last 30 years where a large change came from an existing organization that understood the system.”
“Health v8 2050
Consumers as CEO's of their health!
Data, biomarkers, images frequently, quantitative physicals
Care fully personalized to "one", not for the "average", not population
Predict cancer or disease; predict food/supplement optimization
Al physicians: primary care, psychiatrist, oncologist, cardiologist,...
Obsolescence of symptom based diagnosis (except trauma?)
Healthcare more affordable, accessible, & better quality”
KV Portfolio
Risk bearing: Oscar, Lumiata
Consumer: Carrot, Color, Whole Biome, Viome, MD Algorithms
Clinical Care: Ginger.io, Alivecor, Forward, Curai, Totemic, Ellipsis, Flow
Diagnostics: Guardant, Genalyte, Two Pore, Karius, Inflammatix, Avena, Neurotrack
Imaging: Bay Labs, Heartvista, Zebra, Q.bio, Openwater
Food: Whole Biome, Impossible, Hampton, Ripple, Miraculex, Ukko
Microbiome: Siolta, Viome, Whole Biome
Medical Science: DiscernDX, Scipher, EDITAS, Ukko, eGenesis, Eligo
Other: Deep Genomics, Ultima, Apton, Loop, Vicarious, Atomwise, Healthtap, eGenesis...
[I pretty much always find myself in full agreement with Vinod’s prediction of where healthcare is going. His prediction that 80% of the work clinicians do today can be replaced has always seemed quite a reasonable estimate, it actually probably could be higher.]
18.2 Future of Work
Jennifer Radin, Deloitte
William Morris MD Associate Chief Information Officer, Cleveland Clinic
Shawna Butler RN MBA Nurse Economist and EntrepreNURSE-in-Residence at Radboud University Medical Center
What is the future of work? …the Robot Apocalypse
Longer lifespans - what does a 60-70 year long career look like?
Who does the work (the right person) x
Where is work performed (the right format, the right time) x
How work is performed (doing the right work)
= Value Transformation (efficient, leveraged, collaborative)
Session 19
Care Reimagined; Connected, Digital and Virtualized
19.1 Jay Parkinson
MD Founder & CEO, Sherpaa
Time.
There has been exponential growth in the ways that people can communicate. But no change in the way that physicians can bill their time.
"Healthcare tried to change with by introducing ‘video visits’. Why are we doing this?
a) a 10 minute video visit is similar to a 10 minute office visit
b) Doctors assumed a need to visualize
c) Healthcare has a long history of designing around doctor’s whims and the FFS business model rather than what patients want”
Telehealth in perspective:
~3 million doctor office visits per day in America
~300,000 urgent care visits per day
~3,000 phone/video visits per day
Stats from Kaiser Permanente:
(Kaiser said, about half of their patient interactions are ‘virtual’)
Per year:
20 million email collaborations
17 million online prescription refills
4 million scheduled appointments done online
37 million tests viewed online
From 2015 to 2017:
210,000 total video visits scheduled
152,809 patients chose a video visit
1.25% of 12.2 million patients
Source: NEJM October 11, 2018
An the number of video visits has plateaued off…
What would healthcare look like if we built care services around these cultural changes and brought them to the doctor-patient relationship?
1. One simple online place to go to get care
2. Build a robust online service on par with the capability of urgent care and office-based PCPs
2a. Patient writes their symptoms into free text box
2b. Your doctor (the same doctor) reads the story, reviews the submitted photos, and responds with a broad set of symptom-based questions. Note: all the questions are free text.
2c. If needed your doctor may order some labs or imaging.
2d. Those results come into the conversation of that episode of care.
2e. If medication needed, you enter your zip code, and a pharmacy is confirmed.
2f. If need to see a specialist, you go to them, and then their report is sent back to your clinician (into that conversation thread) for you to read. Their report is imported as a digital fax.
2g. Then you can log back in afterwords and see exactly what the doctor told you
2h. Then the doctor may check in with you after to see how you are doing.
“As patients forget 85% of what they are told in the exam room, it means I’m 15% effective at my job”
Why this works: Synchronous vs Asynchronous Conversations
Ubiquitous asynchronous digital communication - as important as the printing press
Synchronous Conversations:
Exam room conversations - 1.1 billion per year
Phone calls - decreasing
Doctor-patient video chats ~5,000 a day
Asynchronous conversations
Email - tens of billions per day
Text - tens of billions per day
WhatsApp, Facebook Messenger - tens of billions per day
synchronous communication: the process is very linear, and linear process are prone to bottlenecks. (eg. if you take longer with one patient, everyone else has to wait in the waiting room).
Asynchronous communicated - processes are branched and hyperefficient - like triaging your inbox
synchronous: conversations need to be documented
asynchronous: the communication is the documentation
synchronous: itss almost impossible to standardize oral real-time conversations
asynchronous: communication can be standardized taking and communicating care plans
Synchronous: the office visit is a tiny snapshot in an ongoing story
Asynchronous: quick communication snippets enable more frequent, more insightful, higher “touch” care
Synchronous: every conversation is deemed important enough to call a meeting. “Healthcare is like you showed up to a new job, and they said ‘we don’t really believe in e-mail here, everything has to be done in a meeting’”
Asynchronous: most healthcare communication does not require the intensity of an in-person visit
Synchronous: when time is limited, there’s no chance to read up on an unknown case or ask a colleague for their opinion
Asynchronous: '‘I haven’t seen this in a while. I’m going to read up on this and then respond to the patient in the most knowledgeable way.”
Synchronous: “I’ve only got 10 minutes in this visit and don’t know when or if I’ll ever see them again, I better bring out the big guns to protect myself”
Asynchronous: “I have a hunch about what’s going on but this thing will declare itself by tomorrow. I’ll ask you for an update first thing in the morning and then make a decision. But if x, y, or z happen reach back out immediately. Until then, do this to feel better” More conservative practice style.
Synchronous: patient, EMR, fuddling with exam room tools
Asynchronous: triaging messages, responding to messages, hyper-efficient inbox zero kind of work
3. Create a new billing mechanism. The Epsiode of Care
How is this billed - per total length of the episode of care
UTI: 3 days (onset, prescription, check-in, resolution)
Pneumonia 3 weeks (onset, X-ray, prescription, routine check-ins, resolution)
New breast lump 3 months (onset, ultrasound, breast surgeon, check ins, guidance, etc)
95% of all primary / urgent care Episodes of Care (~1500 conditions) can be diagnosed and treated by virtual PCPs without in-person visits
95% of episodes are just messaging + photos
5% involve a phone call
24/7 for urgent access for urgent issues
12 minute response time fro messages within the app
Online you can: ask questions, order tests, collect data (vitals increasingly so with home tools), experiment with treatments, and watch and wait to observe clinical course.
There are increasing new proxy’s for those issues that have a high reliance on a physical exam. Eg. ResApp for pneumonia - cough into app and it gives risk prediction.
Problem of current ‘in-person’ healthcare
What if 80% of the time you show up, and you meet one of their assistants? [Do you think that patients are impressed with this type of care?]
New flavours of relationship are unlocked by new ways to communicate and share.
“Have you ever befriended someone on Facebook or Twitter and never met them, but two years latter feel like you know them? Its kind of like that.
Traditional doctor was associated with a physical neighbourhood. If you moved. You’re out of luck.
Types of patients
The power users 10%, spend $5,000+ per year
The user 20% $1,00-$4,999
Kinda-Healther 30% $200-$999
Super-Healther 40% spend less than $200 per year
***
“So ~95% of problems for 80-90% of people in America could be exclusively solved via Episodes of Care without in-person visits?
Yes.”
****
Change is hard
“The doctor-patient relationship, at it’s core, is just two humans communicating.
But we’ve seen over the last 20 years that the companies that make communication between humans far easier, win.
And they win big and change what it means to be a human”
19.2 Lara Jana
MD Pediatrician, Associate Professor, Penn State
Shifting to prevention, shifts care ‘upstream’. Meaning it gets to paediatrics.
Meaning for babies/children: health, nutrition, safe environment, early stimulation, nurturing adults.
85% of brain growth is in first 3 years.
Adverse Childhood Events
19.3 Walter Greenleaf
AR & VR Thought Leader
Note, when he references VR - he means everything, VR, AR, MR, XR, etc
Growth of VR is expected to be faster than internet or iPhone
Medicine will be the enterprise sector that brings VR into the public sector.
1984, first got involved. At that time the computers were the size of refrigerators.
Being used throughout healthcare…
VR for diagnostic assessments, people to do a task and study their behavior
Your future self: powerful tool that has been shown to help change habits. Create an avatar of yourself to coach you. The avatar can also change / age and look different based on your decisions.
When we get 5G cellular, the data can be live streamed to the device, and this will shrink the size of the processing power required on the device because more can be done in the cloud.
VR can accelerate learning 2x because of ability to create flow state while learning.
19.4 Justin Barad
MD Founder & CEO, OssoVR
Problem in surgical training: too much to learn, too little time to learn it.
Introduction of work hour restrictions (80hr/week) -> lead to loss of ~500 hands on surgical cases - equivalent to about 1 year of training
50% of time is spent with EHR and service related tasks
eg. Anterior Total Hip Replacement - requires 100 surgeries to know it safely. Need even more time to learn robotics.
As proof - research shows 30.7% of graduates couldn’t operate independently despite completing training.
Session 20
Radical Interoperability
John Mattison MD Chief Medical Information Officer, Kaiser Permanente
Patients will want to be able to ask a chatbot anything about their health, and in order to do this the chatbot will require radical interoperability in access to the patient’s entire past medical history.
This is argument for personal cloud for each person.
There will be financial return for use of their medical record. Startups doing this are using blockchain.
John Nebeker MD MS Deputy CMIO, Veterans Health Administration
Seamless care = human experience. That is what patients care about.
Patient’s don’t care about ‘interoperability’ that is a ‘computer experience.
Perversity of the regulations is the #1 problem. We should focus on the goals, not the how.
Shannon Sartin Executive Director, Digital Services, U.S. Department of Health and Human Services
Help bring external talent into healthcare.
Session 21
Lessons in Leadership
Jason Tuschen & Jason Torey Former Navy SEALs, Randori Tech
Part of reason they founded their company is that it is a tragedy for a company with a great idea to fail because of a fixable problem, such as poor leadership.
At the end of training, you have someone who has humbleness, because they acknowledge they have found their Achilles heal; but they also have confidence because he knows he has mental toughness and a team of people behind him to overcome any obstacle.
People often want to know the why for something to be done, and this is important to ensure it’s known. Though, sometimes the leader becomes the why / the inspiration that brings the group together to accomplish a task.
Session 22
Reshaping Pharma, Discovery & Trials
22.1 Noah Craft
MD PhD CEO & Founder, Science 37
Cool company, creating a distributed, decentralized, clinical trial platform built around patients.
The slide deck tells the story:
22.2 Mei Mei Hu
CEO & Co-Founder, United Neuroscience
How can you prevent Alzheimers? Some people seem to age without it. Could you be vaccinated against Alzheimers?
22.3 Onno Faber
Founder, RDMD
Diagnosed with NF2 Mutation - causes benign tumours in the nervous system - problem is the physical growth of them impair nerve function. No treatment available.
Organized a hackathon to work on NF2.
1 in 10 people around the world have a rare disease. (100s of millions of people)
7000 rare disease. Only 5% have a treatment.
Goal: to accelerate the development of treatments for rare disease
MEDy Awards
Zeto - new EEGs
CloudMedx - AI bot to talk with patients
Alavita - spirometry values as a surrogate masure for heart failure “mouthLab”
Seqster - EHR data aggregation platform
You may be interested in the Notes from Day 1, or Notes from Day 2, or Notes from Day 4.
All slides are from the Singularity University’s Exponential Medicine Conference YouTube live stream November 6, 2018.
Watch past Singularity University videos on their channel.
To register for next year’s conference, please visit their website, https://exponential.singularityu.org/medicine/ It sells outs, so register early.
You may be interested in the Notes from Day 1, or Notes from Day 2, or Notes from Day 4.